Metabolic dysfunction–associated steatotic liver disease
It is also associated with hormonal disorders (panhypopituitarism, hypothyroidism, hypogonadism, polycystic ovary syndrome), persistently elevated transaminases, increasing age, and hypoxia caused by obstructive sleep apnea; some of these conditions predict disease progression.
[47] A prospective cohort study found the association between habitual snoring and MASLD development to be significant, and the trend was noted to be most prominent in lean individuals.
Various definitions exist for an inflammatory focus, but one defines it as the presence of more than four mononuclear cells in close proximity inside the hepatic parenchyma.
[56] Based on gene knockout studies in murine models, it has been suggested that, among many other pathogenic factors, TGF beta signals may be crucially involved in promoting the progression of NASH.
In insulin-resistant adipose tissue, such as in people with obesity and type 2 diabetes, more triglycerides are broken down into FFAs and released into the bloodstream, promoting uptake by the liver.
[20] Instead, alteration of the profile of the other lipid subtypes present in the liver, such as diacylglycerols, phospholipids, ceramides, and free cholesterol, have a more significant role in the pathogenesis of MASLD.
NASH represents a more advanced stage of NAFL and is associated with poor outcomes such as cardiovascular events, cirrhosis, or hepatocellular carcinoma.
In people with fatty liver with associated inflammatory injury (steatohepatitis) blood tests are usually used to rule out certain types of viral hepatitis and autoimmune diseases.
[70] The European Association for the Study of the Liver (EASL) recommends screening for steatosis whenever NAFLD is suspected as this is a strong predictor of the disease evolution and predicts future type 2 diabetes, cardiovascular events, and hypertension.
[70] Magnetic resonance elastography (MRE) is an established method that can accurately assess hepatic fibrosis and is recommended by the APASL, AGA, ACR and AASLD.
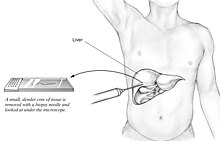
[70] Routine liver function blood tests are not sensitive enough to detect MASLD, and biopsy is the only procedure that can reliably differentiate NAFL from NASH.
[13][88] The Mediterranean diet also showed promising results in a 6-week study with a reduction of NASH induced inflammation and fibrosis, independently from weight loss.
[5][13][66] The Asia-Pacific Work Group advises that Vitamin E may improve liver condition and aminotransferase levels, but only in adults without diabetes or cirrhosis who have NASH.
[14] The NICE guidelines recommend Vitamin E as an option for children and adults with NAFLD with advanced liver fibrosis, regardless of whether the person has diabetes mellitus.
[5][14][103][needs update] Treatment with medications is primarily aimed at improving liver disease and is generally limited to those with biopsy-proven NASH and fibrosis.
[5][14] Indeed, the side effects associated with thiazolidinedione medications, which include osteopenia, increased fracture risk, fluid retention, congestive heart failure, bladder cancer, and long-term weight gain, have limited their adoption.
[5] The NICE provides similar guidelines to the AASLD regarding pioglitazone and recommends it be administered in secondary care to adults with advanced liver fibrosis irrespective of whether or not they have diabetes.
[66] Glucagon-like peptide-1 receptor agonists (GLP-1s) are at least as effective as pioglitazone and Vitamin E and significantly reduce steatosis, ballooning necrosis, lobular inflammation, and fibrosis according to a 2023 systematic review.
[113] In July 2024, two recent papers explore the metabolic effects of GLP-1 receptor agonists can be enhanced by combining them with other incretin hormones or molecules affecting complementary pathways.
Bariatric surgery is an effective method for obese and diabetic individuals with MASLD to induce weight loss and reduce or resolve NASH inflammation, including fibrosis, and improve longevity.
[14] For these reasons and others, individuals with morbid obesity (BMI ≥ 40 kg/m2) and NASH with cirrhosis may be considered unfit for liver transplantation until they follow lifestyle modifications to reduce bodyweight.
[5] MASLD is a risk factor for fibrosis, hypertension, chronic kidney disease, atrial fibrillation, myocardial infarction, ischemic stroke, and death from cardiovascular causes based on very-low to low-quality evidence from observational studies.
[25] MASLD incidence is rapidly rising, along with obesity and diabetes, and has become the most common cause of liver disease in developed countries, for adults, teenagers, and children.
[145] The name "non-alcoholic steatohepatitis" (NASH) was later defined in 1980 by Jurgen Ludwig and his colleagues from the Mayo Clinic[146] to raise awareness of the existence of this pathology, as similar reports previously were dismissed as "patients' lies".
[147][148] Diagnostic criteria began to be worked out, and in 2005 the Pathology Committee of the NIH NASH Clinical Research Network proposed the NAS scoring system.
[25][152][153] MASLD is associated with metabolic syndrome, which is a cluster of risk factors that contribute to the development of cardiovascular disease and type 2 diabetes mellitus.
[5] The EASL suggests using fibrosis tests such as elastography, acoustic radiation force impulse imaging, and serum biomarkers to reduce the number of biopsies.
[28] Intensive lifestyle modifications, including physical activity and dietary changes, are the first line of treatment according to AASLD and EASL as it improves the liver histology and aminotransferase levels.
[34][162] The search for these biomarkers of MASLD, NAFL, and NASH involves lipidomics, medical imaging, proteomics, blood tests, and scoring systems.
[34] According to a review, proton density fat fraction estimation by magnetic resonance imaging (MRI-PDFF) may be considered the most accurate and even gold standard test to quantify hepatic steatosis.