Liver cancer
[7] Higher rates of liver cancer occur where hepatitis B and C are common, including Asia and sub-Saharan Africa.
[3] For example, it is recommended that people with chronic liver disease who are at risk for hepatocellular carcinoma be screened every 6 months using ultrasound imaging.
[16] In terms of HCC diagnosis, it is recommended that people with risk factors (including known chronic liver disease, cirrhosis, etc.)
If the ultrasound shows a focal area that is larger than 1 centimeter in size, patients should then get a triple-phase contrast-enhanced CT or MRI scan.
[21] Risk factors for development of intrahepatic CCA include opisthorchus viverrini infection, Clonorchis sinensis infection, sclerosing cholangitis, choledochal cysts, past procedures of the biliary tree, exposure to thorotrast and dioxins, and cirrhosis.
They are also hard to diagnose but are typically suspected on CT or MRI scans that show focal lesions with differing amounts of signal intensity (these tumors have a lot of bleeding or hemorrhage and subsequent dying of tissue (necrosis)).
The Children's Oncology Group (COG) has developed a protocol to help diagnose and manage childhood liver tumors.
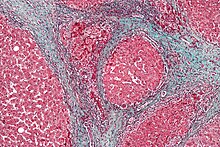
[32] HBV and HCV can lead to HCC, because these viral infections cause massive inflammation, fibrosis, and eventual cirrhosis occurs within the liver.
NASH and NAFL is beginning to be called a risk factor for liver cancer, particularly HCC.
For HCC these include medical ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI).
[17] Sometimes doctors will get a liver biopsy, if they are worried about HCC and the imaging studies (CT or MRI) do not have clear results.
[17] The majority of cholangiocarcimas occur in the hilar region of the liver, and often present as bile duct obstruction.
High levels of alpha-fetoprotein (AFP) in the blood can be found in many cases of HCC and intrahepatic cholangiocarcinoma.
[17] Of note, AFP is most useful for monitoring if liver cancers come back after treatment rather than for initial diagnosis.
Primary prevention preemptively reduces exposure to a risk factor for liver cancer.
[55] Aflatoxin exposure can be avoided by post-harvest intervention to discourage mold, which has been effective in west Africa.
Cure of virus-infected individuals is not possible, but treatment with antiviral drugs can decrease the risk of liver cancer.
There are many chemotherapeutic drugs approved for liver cancer including: atezolizumab, nivolumab, pembrolizumab, regorafenib.
[61] Recent advances in liver cancer treatment are exploring T cells engineered with chimeric antigen receptors (CARs) targeting glypican-3 (GPC3), such as GAP T cells, showing potential in addressing GPC3-positive tumors, especially in pediatric liver cancers.
[62][63] Partial surgical resection is the recommended treatment for hepatocellular carcinoma (HCC) when patients have sufficient hepatic function reserve.
Systemic chemotherapeutics are not routinely used in HCC, although local chemotherapy may be used in a procedure known as transarterial chemoembolization (TACE).
In this procedure, drugs that kill cancer cells and interrupt the blood supply are applied to the tumor.
Because most systemic drugs have no efficacy in the treatment of HCC, research into the molecular pathways involved in the production of liver cancer produced sorafenib, a targeted therapy drug that prevents cell proliferation and blood cell growth.
The reason the majority of intrahepatic cholangiocarcinomas are not able to be surgically removed is because there are often multiple focal tumors within the liver.
[46] 60% of cholangiocarcinomas form in the perihilar region and photodynamic therapy can be used to improve quality of life and survival time in these un-resectable cases.
[46] Radio frequency ablation, transarterial chemoembolization and internal radiotherapy (brachytherapy) all show promise in the treatment of cholangiocarcinoma[72] and can sometimes improve bile flow, which can decrease the symptoms a patient experiences.
[10] Estimates based on most recent data suggest that each year there are 841,000 new liver cancer diagnoses and 782,000 deaths across the globe.
[55] In terms of gender breakdown, globally liver cancer is more common in men than in women.
Cholangiocarcinoma also has a significant geographical distribution, with Thailand showing the highest rates worldwide due to the presence of liver fluke.
[79] In terms of mortality, the 5-year survival rate for liver and intrahepatic bile duct cancers in the United States is 19.6%.