Occipital epilepsy
Epileptic seizures are the result of synchronized neural activity that is excessive, and may stem from a failure of inhibitory neurons to regulate properly.
There may be no known cause of this type of seizure, but these epilepsies may occur for a variety of reasons, such as brain tumors, infection, trauma and lesions, and idiopathic onset.
Since the event is located in the occipital lobe, symptoms may occur spontaneously and include visual stimuli.
Calcarine fissure- inferior tends to spread to the temporal lobe and superior can spread to the parietal, fronto-parietal operculum, or frontal lobes[7] Also referred to as ICOE-G, this type primarily affects vision and may cause partial vision loss, a sensation of flashing lights, multi-colored spots and shapes, hallucinations (rare), jerking on one side of the body, and headaches during or after the seizure.
[2] The main seizure type of this classification of occipital epilepsy is known as autonomic due to the symptoms experienced such as turning pale, feeling ill, and usually vomiting, dilation of pupils, sweating, drooling, and watering of the eyes.
Interestingly, over two-thirds of these seizures occur during sleep, whether it be at night or during a daytime nap, but usually are not very frequent- typically one or two every few months.
Lesions can be due to occipital cortical dysplasia, which can be difficult to identify and diagnose based on an MRI.
A seizure occurs when this communication is disrupted, and the brain area receives a burst of abnormal electrical signaling, interrupting the normal function.
The disorder of electrical signals causes excessive excitation or loss of inhibition, which is a function of malfunctioning ion channels, as neurotransmitters are released in an unorganized fashion.
If a specific region is where the seizure is located, the brain will continue to try to make changes in that area, causing increased symptoms for that individual.
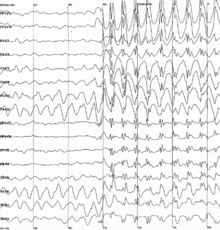
[9] Procedures for diagnosis of occipital epilepsy include hematology, biochemistry, screenings for metabolic disorders, DNA analysis, and most commonly, MRI.
The detailed mechanism of epilepsy has not been completely understood, but various anti-epileptic drugs can have a significant effect in reducing symptoms.
These work by taking action on voltage-dependent sodium, calcium, and potassium channels, as well as GABA and excitatory receptors, various enzymes, and synaptic proteins.
The frequency of seizures, the severity of damage and symptoms, and the individual's response to treatment can vary from a relatively good outlook to a progressive decline.
For many children with one of these types of occipital epilepsy, it is possible to live a normal adult life and to wean off of their anti-epileptic drugs.
For brain function, most occipital epilepsy patients have normal experiences throughout their education, although a few may have minor difficulties with learning.
[14] Scientists are also trying to determine a more clear differential in diagnosis of occipital epilepsy, specifically distinguishing it from migraines.
[15] In migraines, the visual symptoms usually begin with a small sparkling, shimmering area that expands slowly, and often has jagged edges.
They concluded that dysfunction in visual and spatial organization is related to OE diagnosis, and supports disruption in the occipito-parietal stream.