Osteoporosis
[4] Prevention of osteoporosis includes a proper diet during childhood, hormone replacement therapy for menopausal women, and efforts to avoid medications that increase the rate of bone loss.
[109] In addition to the detection of abnormal BMD, the diagnosis of osteoporosis requires investigations into potentially modifiable underlying causes; this may be done with blood tests.
Depending on the likelihood of an underlying problem, investigations for cancer with metastasis to the bone, multiple myeloma, Cushing's disease and other above-mentioned causes may be performed.
However, radiography is relatively insensitive to detection of early disease and requires a substantial amount of bone loss (about 30%) to be apparent on X-ray images.
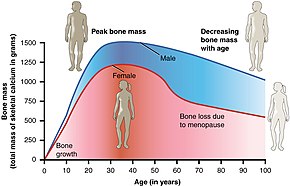
Osteoporosis is diagnosed when the bone mineral density is less than or equal to 2.5 standard deviations below that of a young (30–40-year-old[4]:58), healthy adult women reference population.
[4]:58 The World Health Organization has established the following diagnostic guidelines:[4][27] The International Society for Clinical Densitometry takes the position that a diagnosis of osteoporosis in men under 50 years of age should not be made on the basis of densitometric criteria alone.
Among QCT's advantages: it can be performed at axial and peripheral sites, can be calculated from existing CT scans without a separate radiation dose, is sensitive to change over time, can analyze a region of any size or shape, excludes irrelevant tissue such as fat, muscle, and air, and does not require knowledge of the patient's subpopulation in order to create a clinical score (e.g. the Z-score of all females of a certain age).
Among QCT's disadvantages: it requires a high radiation dose compared to DXA, CT scanners are large and expensive, and because its practice has been less standardized than BMD, its results are more operator-dependent.
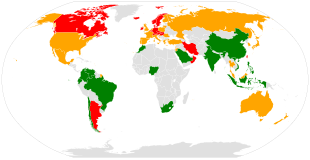
[118] The U.S. Preventive Services Task Force (USPSTF) recommend that all women 65 years of age or older be screened by bone densitometry.
[125] In people with coeliac disease adherence to a gluten-free diet decreases the risk of developing osteoporosis[126] and increases bone density.
[65] The diet must ensure optimal calcium intake (of at least one gram daily) and measuring vitamin D levels is recommended, and to take specific supplements if necessary.
[128] These individuals should also be intentional about intaking an adequate amount of protein, calcium, and vitamin D. If the woman has an even higher risk of fracture, managing this may require therapy.
[131] The USPSTF does not recommend low dose supplementation (less than 1 g of calcium and 400 IU of vitamin D) in postmenopausal women as there does not appear to be a difference in fracture risk.
[144] Weight bearing exercise has been found to cause an adaptive response in the skeleton,[145] promoting osteoblast activity and protecting bone density.
[151] Risk of adverse events from the types of exercise usually considered appropriate for people with osteoporosis is generally low (though repeated forceful forward spinal bends are discouraged).
[153] Osteoporosis is a very prevalent disease in the elderly population but not much is known about the optimal prescription and dosage of physical exercise to help prevent bone mineral loss.
Important things often overlooked when treating osteoporosis are muscle strength and maintenance of BMD, which should be incorporated into the program to optimize the benefits of exercise.
Recommended dosage for progressive resistance training is 2 or more days a week, intensity (load) should start low and increase gradually.
Resistance training exercises, like weight lifting, can lead to brief increased in anabolic hormones, like testosterone, which aid in muscle and bone strength.
[163] The increase in mechanical tension during resistance exercise will likely help stimulate the production of Insulin-like growth factors in the bone, but at a greater extent.
[164] Research suggest that regular resistance training accompanied with weight-bearing activities help reduce the progression of osteoporosis and risk of fracture.
[178] Fluoride supplementation does not appear to be effective in postmenopausal osteoporosis, as even though it increases bone density, it does not decrease the risk of fractures.
Romosozumab is usually reserved for patients with very high fracture risk and is the only available drug therapy for osteoporosis that leads to simultaneous inhibition of bone resorption together with an anabolic effect.
[185][186] Certain medications like alendronate, etidronate, risedronate, raloxifene, and strontium ranelate can help to prevent osteoporotic fragility fractures in postmenopausal women with osteoporosis.
Hip fractures can lead to decreased mobility and additional risks of numerous complications (such as deep venous thrombosis and/or pulmonary embolism, and pneumonia).
[190] Vertebral fractures, while having a smaller impact on mortality, can lead to severe chronic pain of neurogenic origin, which can be hard to control, as well as deformity.
Though rare, multiple vertebral fractures can lead to such severe hunchback (kyphosis), the resulting pressure on internal organs can impair one's ability to breathe.
[13][16] This places a large economic burden on the healthcare system due to costs of treatment, long-term disability, and loss of productivity in the working population.
[206] Anthropologists have studied skeletal remains that showed loss of bone density and associated structural changes that were linked to a chronic malnutrition in the agricultural area in which these individuals lived.
"It follows that the skeletal deformation may be attributed to their heavy labor in agriculture as well as to their chronic malnutrition", causing the osteoporosis seen when radiographs of the remains were made.