Palpitations
This article will explore the potential causes of palpitations, from benign triggers to more serious underlying cardiac conditions.
This article will also discuss the key steps in evaluating palpitations, including history-taking, physical exams, and diagnostic tests, as well as the various treatment approaches based on the underlying causes.
If a benign cause for these symptoms isn't found at the first visit, then prolonged heart monitoring at home or in the hospital setting may be needed.
Noncardiac symptoms should also be elicited since the palpitations may be caused by a normal heart responding to a metabolic or inflammatory condition.
Hyperventilation, hand tingling, and nervousness are common when anxiety or panic disorder is the cause of the palpitations.
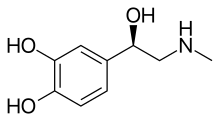
[1] In one study reporting the etiology of palpitations, 43% were found to be cardiac, 31% psychiatric, and approximately 10% were classified as miscellaneous (medication induced, thyrotoxicosis, caffeine, cocaine, anemia, amphetamine, mastocytosis).
[1] Supraventricular tachycardias can also be induced at the termination of exercise when the withdrawal of catecholamines is coupled with a surge in the vagal tone.
[1] Palpitations secondary to catecholamine excess may also occur during emotionally startling experiences, especially in patients with a long QT syndrome.
[1] Anxiety and stress elevate the body's level of cortisol and adrenaline, which in turn can interfere with the normal functioning of the parasympathetic nervous system resulting in overstimulation of the vagus nerve.
The link between anxiety and palpitation may also explain why many panic attacks involve an impending sense of cardiac arrest.
Similarly, physical and mental stress may contribute to the occurrence of palpitation, possibly due to the depletion of certain micronutrients involved in maintaining healthy psychological and physiological function.
[citation needed] Many psychiatric conditions can result in palpitations including depression, generalized anxiety disorder, panic attacks, and somatization.
[1] There are many metabolic conditions that can result in palpitations including, hyperthyroidism, hypoglycemia, hypocalcemia, hyperkalemia, hypokalemia, hypermagnesemia, hypomagnesemia, and pheochromocytoma.
[1] The medications most likely to result in palpitations include sympathomimetic agents, anticholinergic drugs, vasodilators and withdrawal from beta blockers.
[1][10] Excessive consumption of caffeine, commonly found in coffee, tea, and energy drinks, is a well-known trigger.
[1] Recreational drugs such as marijuana, cocaine, amphetamines, and MDMA (Ecstasy) are also associated with palpitations and pose significant cardiovascular risks.
[1] To diagnose palpitations, patient description is of notable importance, and a complete history and physical exam are essential.
[1][2] The physical exam should include checking vital signs and a position based blood pressure measurement, listening to the heart and lungs and examining the arms and legs.
[1][4] A harsh holo-systolic murmur best heard at the left sternal border which increases with Valsalva may indicate hypertrophic obstructive cardiomyopathy.
[1] The presence of a short PR interval and a delta wave (Wolff-Parkinson-White syndrome) is an indication of the existence of ventricular pre-excitation.
[1] Significant left ventricular hypertrophy with deep septal Q waves in I, L, and V4 through V6 may indicate hypertrophic obstructive cardiomyopathy.
[1] An aggressive diagnostic approach is recommended for those at high risk and can include ambulatory monitoring or electrophysiologic studies.
[1] Electrophysiology testing enables a detailed analysis of the underlying mechanism of the cardiac arrhythmia as well as the site of origin.
[2] These maneuvers involves holding one's breath and bearing down—can be employed to stimulate the vagus nerve and slow the heart rate.
[13] However, these techniques may provide only temporary relief, and if palpitations persist or are associated with other concerning symptoms, medical evaluation is essential to determine any underlying causes and appropriate treatment options.
[1] However, patients with palpitations linked to fainting (syncope), uncontrolled arrhythmias, poor blood flow (hemodynamic issues), or chest pain (angina) should get further evaluation.
To treat this type of palpitation, the cause of irritation to the vagus nerve or parasympathetic nervous system needs to be found and fixed.
[14] Formal research has found that current smartwatch apps can detect abnormal heart rhythms, like atrial fibrillation and alert people to this.
[1] Following up with a primary care doctor can help track symptoms and decide if a heart specialist (cardiologist) is needed.
[1] There are four types of sensations: Extra-systolic (premature heartbeats), Tachycardic (rapid heart rate), Anxiety-related or Intense palpitations.