Pathology of multiple sclerosis
At least five characteristics are present in CNS tissues of MS patients: Inflammation beyond classical white matter lesions (NAWM, NAGM), intrathecal Ig production with oligoclonal bands, an environment fostering immune cell persistence, Follicle-like aggregates in the meninges (B-cells mostly infected with EBV[4]) and a disruption of the blood–brain barrier even outside of active lesions.
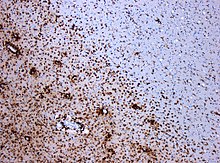
[9] A combination of histologic and/or immunohistochemical stains can be used to visualize post-mortem MS characteristic lesions and to diagnose post-mortem "inflammatory demyelinating lesions consistent with MS":[12] These markers are specific for the different processes that drive the formation of plaques: inflammation, myelin breakdown, astrogliosis, oligodendrocyte injury, neurodegeneration, axonal loss and remyelination.
[15] In some cases (pattern II), a special subset of lymphocytes, called T helper cells or "CD4+ T-cells" play a key role in the development of the lesion in a way similar to the CD4+ attacks that appear in anti-MOG associated encephalomyelitis.
Recent research as of 2019 point to one of the HERV-W viruses (pHEV-W), and specifically one of the proteins of the viral capside that has been found to "activate microglia" in vitro.
[24] Supporting this study, a monoclonal antibody against the viral capside (Temelimab) has shown good results in trials in phase IIb.
Repeated attacks lead to successively fewer effective remyelinations, until a scar-like plaque is built up around the damaged axons.
[34] The distribution of the lesions could be linked to the clinical evolution[35] Post-mortem autopsy reveal that gray matter demyelination occurs in the motor cortex, cingulate gyrus, cerebellum, thalamus and spinal cord.
Regarding two parameters of the cortical lesions (CLs), fractional anisotropy (FA) is lower and mean diffusivity (MD) is higher in patients than in controls.
MS cord pathology is independent of brain changes, develops at different rates according to disease phenotype, and is associated to medium-term disability accrual.
[60] Recently it has been found that Normal Appearing Cortex presents primary neurodegenerative damage in the dendritic spines of the neurons, with no demyelination nor autoimmune infiltrates.
Related to this, the CSF of patients with disease activity show high levels of "Lateral Olfactory Tract Usher Substance" (LOTUS)[64] The eye's retina in MS is also damaged.
[65] The retina and the optic nerve originate as outgrowths of the brain during embryonic development, so they are considered part of the central nervous system (CNS).
[70] This measure can be used to predict disease activity[71] and to establish a differential diagnosis from Neuromyelitis optica[72] About antibodies in the retina, tissue-bound IgG was demonstrated on retinal ganglion cells in six of seven multiple sclerosis cases but not in controls.
[73] Two eye problems, Uveitis and retinal phlebitis are manifestations of MS.[74] Proposed procedures for the neurodegeneration are than Narrower arterioles and wider venules have been reported.
[84] A relationship between neural damage and N-Acetyl-Aspartate concentration has been established, and this could lead to new methods for early MS diagnostic through magnetic resonance spectroscopy.
The collaboration between LTB on Th17 cells and LTBR (Lymphotoxin beta receptor) on meningeal radio-resistant cells is very crucial for the induction and progression of MS.[88] Follicle-like aggregates in the meninges are formed only in secondary progressive MS.[89] and correlate with the degree of subpial cortical demyelination and brain atrophy, suggesting that they might contribute to cortical pathology in SPMS[89] These ectopic lymphoid follicles are composed mainly of EBV infected B-cells.
[90] Though MS is defined as a CNS condition, some reports link problems in the peripheral nervous system with the presence of MS plaques in the CNS[91] Currently, a new disease entity, combined central and peripheral demyelination has been defined as the simultaneous demyelination of the periferal and central nervous systems.
It can be seen that before the BBB breakdown, this coefficient increases until, at some point, the blood-brain barrier breaks down and immune cells enter the brain producing the lesion.
[100] A fourth area called DAWM (diffusely abnormal white matter) has been proposed[116] and can help to differentiate PPMS and SPMS.
[117] Abundant extracellular myelin in the meninges of patients with multiple sclerosis has been found[118] Brain tissues with MRI-hidden problems are usually named Normal Appearing.
[141][142] The earliest change reported in the lesions examined is widespread oligodendrocyte apoptosis in which T cells, macrophages, activated microglia, reactive astrocytes, and neurons appear normal.
White matter lesions appear in NAWM areas,[22] and their behavior can be predicted by MRI parameters as MTR (magnetization transfer ratio).
[151] It also seems that myelin basic protein (MBP) from multiple sclerosis (MS) patients contains lower levels of phosphorylation at Thr97 than normal individuals.
[162] Changes in the vasculature take place not only in focal lesions but also in DAWM as detected by postmortem MRI[163] Dirty-appearing white matter (referred to as DAWM like the former case) is defined as a region with ill-defined borders of intermediate signal intensity between that of normal-appearing white matter (NAWM) and that of plaque on T2-weighted and proton density imaging.
[168] For some authors, what we call MS in reality is a heterogeneous group of diseases[169] Some independent reports take also PPMS apart[170] Some others point a connection between some MS cases and peripheral neuropathies[171] Some reports propose the existence of molecular biomarkers that determine the clinical course of the disease,[172] but the relationship to the pathological types has still not been established as of 2016.
[192] Nevertheless, after some debate among research groups, the four patterns model is accepted and the exceptional case found by Prineas has been classified as NMO[193][194] For some investigation teams this means that MS is a heterogeneous disease.
As in relapsing MS also in progressive MS active tissue injury is invariably associated with inflammation, but inflammation seems to be trapped behind a closed blood brain barrier[229] A specially remarkable difference between PPMS and SPMS are some follicle-like B-cells structures in the meninges of SPMS patients, that have never been reported in PPMS patients.
Ectopic Follicle-Like Structures, EFS's, or Tertiary Lynphoid Tissues, TLT's) in the meninges that appear associated with underlying subpial cortical damage.
This means that for clinical definite cases, MS condition has been present for a long time, complicating the study of the initial stages.
Oligodendrocytes evolution is similar to normal MS clinical courses[240] Sometimes patients that undergo an MRI examination for an unrelated cause can show lesions in their brains.