Pulse oximetry
Fingertips and earlobes have disproportionately high blood flow relative to their size, in order to keep warm, but this will be lacking in hypothermic patients.
[6] Because of their simplicity of use and the ability to provide continuous and immediate oxygen saturation values, pulse oximeters are of critical importance in emergency medicine and are also very useful for patients with respiratory or cardiac problems,[7] especially COPD, or for diagnosis of some sleep disorders such as apnea and hypopnea.
Portable pulse oximeters are also useful for mountain climbers and athletes whose oxygen levels may decrease at high altitudes or with exercise.
Additional risks for injury include lack of pain response where the probe is placed, such as having an insensate limb, or being unconscious or under anesthesia, or having communication difficulties.
[17] Because pulse oximeter devices are calibrated for healthy subjects, their accuracy is poor for critically ill patients and preterm newborns.
Pulse oximetry technologies differ in their abilities to provide accurate data during conditions of motion and low perfusion.
[8] Some home pulse oximeters have low sampling rates, which can significantly underestimate dips in blood oxygen levels.
[9] Research has suggested that error rates in common pulse oximeter devices may be higher for adults with dark skin color, leading to claims of encoding systemic racism in countries with multi-racial populations such as the United States.
[20][21] The issue was first identified decades ago; one of the earliest studies on this topic occurred in 1976, which reported reading errors in dark-skinned patients that reflected lower blood oxygen saturation values.
[27] Further studies and computer simulations show that the increased amounts of melanin found in people with darker skin scatter the photons of light used by the pulse oximeters, decreasing the accuracy of the measurements.
[28] This inaccuracy can lead to potentially missing people who need treatment, as pulse oximetry is used for the screening of sleep apnea and other types of sleep-disordered breathing,[8] which in the United States are conditions more prevalent among minorities.
[29][30][31] This bias is a significant concern, as a 2% decrease is important for respiratory rehabilitation, studies of sleep apnea, and athletes performing physical efforts; it can lead to severe complications for the patient, requiring an external oxygen supply or even hospitalization.
[32] Another concern regarding pulse oximetry bias is that insurance companies and hospital systems increasingly use these numbers to inform their decisions.
Opinions vary about the reliability of consumer oximeters; a typical comment is "The research data on home monitors has been mixed, but they tend to be accurate within a few percentage points".
[citation needed] When a pulse oximeter is shared between two patients, to prevent cross-infection it should be cleaned with alcohol wipes after each use or a disposable probe or finger cover should be used.
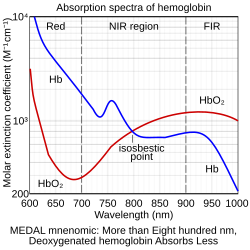
More specifically, it uses light spectrometry to measure what percentage of hemoglobin, the protein in blood that carries oxygen, is loaded.
[citation needed] For a person breathing room air at or near sea level, an estimate of arterial pO2 can be made from the blood-oxygen monitor "saturation of peripheral oxygen" (SpO2) reading.
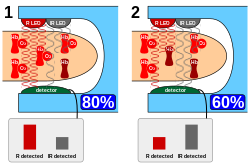
[citation needed] A typical pulse oximeter uses an electronic processor and a pair of small light-emitting diodes (LEDs) facing a photodiode through a translucent part of the patient's body, usually a fingertip or an earlobe.
Due to changes in blood volumes in the skin, a plethysmographic variation can be seen in the light signal received (transmittance) by the sensor on an oximeter.
[52] Motion artifact can be a significant limitation to pulse oximetry monitoring, resulting in frequent false alarms and loss of data.
Perfusion index has been shown to help clinicians predict illness severity and early adverse respiratory outcomes in neonates,[55][56][57] predict low superior vena cava flow in very low birth weight infants,[58] provide an early indicator of sympathectomy after epidural anesthesia,[59] and improve detection of critical congenital heart disease in newborns.
[18][19][61] Signal extraction technology pulse oximetry performance has also been shown to translate into helping clinicians improve patient outcomes.
[63] The measure-through motion and low perfusion capabilities it has also allow it to be used in previously unmonitored areas such as the general floor, where false alarms have plagued conventional pulse oximetry.
[65] In 2007, Masimo introduced the first measurement of the pleth variability index (PVI), which multiple clinical studies have shown provides a new method for automatic, noninvasive assessment of a patient's ability to respond to fluid administration.
[68] Recently, the National Health Service in the United Kingdom and the French Anesthesia and Critical Care Society listed PVI monitoring as part of their suggested strategies for intra-operative fluid management.
[69][70] In 2011, an expert workgroup recommended newborn screening with pulse oximetry to increase the detection of critical congenital heart disease (CCHD).
[72][73] The CCHD workgroup recommended newborn screening be performed with motion tolerant pulse oximetry that has also been validated in low perfusion conditions.
In 2011, the US Secretary of Health and Human Services added pulse oximetry to the recommended uniform screening panel.
[76] High-resolution pulse oximetry (HRPO) has been developed for in-home sleep apnea screening and testing in patients for whom it is impractical to perform polysomnography.
[77][78] It stores and records both pulse rate and SpO2 in 1 second intervals and has been shown in one study to help to detect sleep disordered breathing in surgical patients.