Syphilis
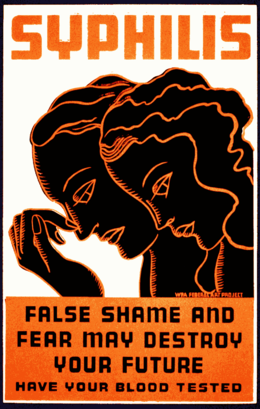
[6][10] After decreasing dramatically with the availability of penicillin in the 1940s, rates of infection have increased since the turn of the millennium in many countries, often in combination with human immunodeficiency virus (HIV).
[19] Approximately 2–6 weeks after contact (with a range of 10–90 days) a skin lesion, called a chancre, appears at the site and this contains infectious bacteria.
[20][21] This is classically (40% of the time) a single, firm, painless, non-itchy skin ulceration with a clean base and sharp borders approximately 0.3–3.0 cm in size.
[21] It may occur early, being either asymptomatic or in the form of syphilitic meningitis; or late as meningovascular syphilis, manifesting as general paresis or tabes dorsalis.
[30] Late symptomatic neurosyphilis can develop decades after the original infection and includes 2 types; general paresis and tabes dorsalis.
[7] Common symptoms that develop over the first couple of years of life include enlargement of the liver and spleen (70%), rash (70%), fever (40%), neurosyphilis (20%), and lung inflammation (20%).
[7] If untreated, late congenital syphilis may occur in 40%, including saddle nose deformation, Higouménakis' sign, saber shin, or Clutton's joints among others.
[35] Syphilis is transmitted primarily by sexual contact or during pregnancy from a mother to her baby; the bacterium is able to pass through intact mucous membranes or compromised skin.
[3] It is not generally possible to contract syphilis through toilet seats, daily activities, hot tubs, or sharing eating utensils or clothing.
[46] The Centers for Disease Control and Prevention (CDC) states, "Correct and consistent use of latex condoms can reduce the risk of syphilis only when the infected area or site of potential exposure is protected.
[50] Several measures to increase access to testing appear effective at reducing rates of congenital syphilis in low- to middle-income countries.
[52] Point-of-care testing to detect syphilis appeared to be reliable, although more research is needed to assess its effectiveness and into improving outcomes in mothers and babies.
Mercury is in fact highly anti-microbial: by the 16th century it was sometimes found to be sufficient to halt development of the disease when applied to ulcers as an inunction or when inhaled as a suffumigation.
[69] Doxycycline and tetracycline are alternative choices for those allergic to penicillin; due to the risk of birth defects, these are not recommended for pregnant women.
[88] According to the Columbian theory, syphilis was brought to Spain by the men who sailed with Christopher Columbus in 1492 and spread from there, with a serious epidemic in Naples beginning as early as 1495.
The difference between rural and urban populations was first noted by Ellis Herndon Hudson, a clinician who published extensively about the prevalence of treponematosis, including syphilis, in times past.
[95] The most compelling evidence for the validity of the pre-Columbian hypothesis is the presence of syphilitic-like damage to bones and teeth in medieval skeletal remains.
[97] In 2020, a group of leading paleopathologists concluded that enough evidence had been collected to prove that treponemal disease, almost certainly including syphilis, had existed in Europe prior to the voyages of Columbus.
Damaged teeth and bones may seem to hold proof of pre-Columbian syphilis, but there is a possibility that they point to an endemic form of treponemal disease instead.
As syphilis, bejel, and yaws vary considerably in mortality rates and the level of human disease they elicit, it is important to know which one is under discussion in any given case, but it remains difficult for paleopathologists to distinguish among them.
Research by Marylynn Salmon has demonstrated that deformities in medieval subjects can be identified by comparing them to those of modern victims of syphilis in medical drawings and photographs.
The association of saddle nose with evil is an indication that the artists were thinking of syphilis, which is typically transmitted through sexual intercourse with promiscuous partners, a mortal sin in medieval times.
It remains mysterious why the authors of medieval medical treatises so uniformly refrained from describing syphilis or commenting on its existence in the population.
Its damage was caused not so much by great sickness or death early in the course of the disease but rather by its gruesome effects decades after infection as it progressed to neurosyphilis with tabes dorsalis.
[112] The first effective treatment for syphilis was arsphenamine, discovered by Sahachiro Hata in 1909, during a survey of hundreds of newly synthesized organic arsenical compounds led by Paul Ehrlich.
During the 20th century, as both microbiology and pharmacology advanced greatly, syphilis, like many other infectious diseases, became more of a manageable burden than a scary and disfiguring mystery, at least in developed countries among those people who could afford to pay for timely diagnosis and treatment.
[114] Many famous historical figures, including Franz Schubert, Arthur Schopenhauer, Édouard Manet,[11] Charles Baudelaire,[115] and Guy de Maupassant are believed to have had the disease.
[117] The earliest known depiction of an individual with syphilis is Albrecht Dürer's Syphilitic Man (1496), a woodcut believed to represent a Landsknecht, a Northern European mercenary.
[118] The myth of the femme fatale or "poison women" of the 19th century is believed to be partly derived from the devastation of syphilis, with classic examples in literature including John Keats' "La Belle Dame sans Merci".
[124] The Public Health Service started working on this study in 1932 in collaboration with Tuskegee University, a historically black college in Alabama.










|
no data
<35
35–70
70–105
105–140
140–175
175–210
|
210–245
245–280
280–315
315–350
350–500
>500
|