Spinal cord injury
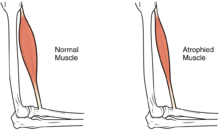
Complications can include muscle atrophy, loss of voluntary motor control, spasticity, pressure sores, infections, and breathing problems.
Research into potential treatments includes stem cell implantation, hypothermia, engineered materials for tissue support, epidural spinal stimulation, and wearable robotic exoskeletons.
[4] Spinal cord injury can be traumatic or nontraumatic,[5] and can be classified into three types based on cause: mechanical forces, toxic, and ischemic from lack of blood flow.
[13] It is based on neurological responses, touch and pinprick sensations tested in each dermatome, and strength of the muscles that control key motions on both sides of the body.
[33] This rare syndrome causes the loss of proprioception and sense of vibration below the level of injury[27] while motor function and sensation of pain, temperature, and touch remain intact.
[35] Tabes dorsalis, due to injury to the posterior part of the spinal cord caused by syphilis, results in loss of touch and proprioceptive sensation.
[10] The effects of injuries at or above the lumbar or sacral regions of the spinal cord (lower back and pelvis) include decreased control of the legs and hips, genitourinary system, and anus.
[6] Signs and symptoms of AD include anxiety, headache, nausea, ringing in the ears, blurred vision, flushed skin, and nasal congestion.
[65] The usual signs and symptoms of DVT and pulmonary embolism may be masked in SCI cases due to effects such as alterations in pain perception and nervous system functioning.
[65] Urinary tract infection (UTI) is another risk that may not display the usual symptoms (pain, urgency, and frequency); it may instead be associated with worsened spasticity.
[52] The use of intermittent catheterization to empty the bladder at regular intervals throughout the day has decreased the mortality due to kidney failure from UTI in the first world, but it is still a serious problem in developing countries.
[86] Falls can be prevented by making changes to the environment, such as nonslip materials and grab bars in bathtubs and showers, railings for stairs, child and safety gates for windows.
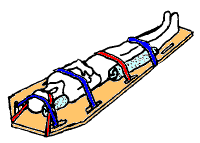
[95] Injuries or fractures in the head, neck, or pelvis as well as penetrating trauma near the spine and falls from heights are assumed to be associated with an unstable spinal column until it is ruled out in the hospital.
[97] Initial care in the hospital, as in the prehospital setting, aims to ensure adequate airway, breathing, cardiovascular function, and spinal motion restriction.
[108] People with cervical or high thoracic injuries may experience a dangerously slowed heart rate; treatment to speed it may include atropine.
[106] Surgery is also necessary when something is pressing on the cord, such as bone fragments, blood, material from ligaments or intervertebral discs,[110] or a lodged object from a penetrating injury.
[112] Recent large-scale studies have shown that patients who do undergo earlier surgery (within 12–24 hours) experience significantly lower rates of life-threatening complications and spend less time in hospital and critical care.
In the acute phase physical therapists focus on the patient's respiratory status, prevention of indirect complications (such as pressure ulcers), maintaining range of motion, and keeping available musculature active.
Physical therapy treatment for airway clearance may include manual percussions and vibrations, postural drainage,[120] respiratory muscle training, and assisted cough techniques.
[124] People with SCI may need to use specialized devices and to make modifications to their environment in order to handle activities of daily living and to function independently.
[29] People with nontraumatic causes of SCI have been found to be less likely to develop complete injuries and some complications such as pressure sores and deep vein thrombosis, and to have shorter hospital stays.
[12] In addition to the completeness and level of the injury, age and concurrent health problems affect the extent to which a person with SCI will be able to live independently and to walk.
[152] The Greek physician Hippocrates, born in the fifth century BC, described SCI in his Hippocratic Corpus and invented traction devices to straighten dislocated vertebrae.
[153] But it was not until Aulus Cornelius Celsus, born 30 BC, noted that a cervical injury resulted in rapid death that the spinal cord itself was implicated in the condition.
[154] The seventh-century Greek physician Paul of Aegina described surgical techniques for treatment of broken vertebrae by removing bone fragments, as well as surgery to relieve pressure on the spine.
[152] Little medical progress was made during the Middle Ages in Europe; it was not until the Renaissance that the spine and nerves were accurately depicted in human anatomy drawings by Leonardo da Vinci and Andreas Vesalius.
[156] In 1934, the mortality rate in the first two years after injury was over 80%, mostly due to infections of the urinary tract and pressure sores,[157] the latter of which were believed to be intrinsic to SCI rather than a result of continuous bedrest.
[77] The former seeks to prevent the harm that occurs from secondary injury in the minutes to weeks following the insult, and the latter aims to reconnect the broken circuits in the spinal cord to allow function to return.
The surgery was performed in Poland in collaboration with Prof. Geoff Raisman, chair of neural regeneration at University College London's Institute of Neurology, and his research team.
In a study published in May 2023 in the journal Nature, researchers in Switzerland described such implants which allowed a 40-year old man, paralyzed from the hips down for 12 years, to stand, walk and ascend a steep ramp with only the assistance of a walker.