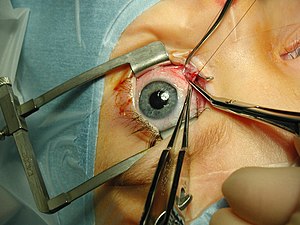
Strabismus surgery
[2] The idea of treating strabismus by cutting some of the extraocular muscle fibers was published in American newspapers by New York oculist John Scudder in 1837.
Surgery is indicated when other, less invasive methods have been unable to treat the misalignment or when the procedure will significantly improve quality of life and/or visual function.
Measured in PD, the size of the deviation is used along with established formulas and tables to inform the surgeon how the muscle must be manipulated in surgery.
[4] Plication has the advantages of being a quicker procedure that involves less trauma than a resection and preserves the anterior ciliary arteries - the latter of which minimizes the risk of blood loss to the front of the eye allowing for operation on multiple muscles at one time.
For example, a recent study compared the outcomes of bilateral lateral rectus recession and unilateral recession/resection of the later/medial recti for intermittent exotropia.
[4] The inferior oblique muscle is rarely tightened due to the technical difficulty of the procedure and the possibility of damage to the macula, which is responsible for central vision.
[citation needed] A relatively new method, primarily devised by Swiss ophthalmologist Daniel Mojon, is minimally invasive strabismus surgery (MISS)[9] which has the potential to reduce the risk of complications and lead to faster visual rehabilitation and wound healing.
A study published in 2017 documented fewer conjunctival and eyelid swelling complications in the immediate postoperative period after MISS with long-term results being similar between both groups.
[10] MISS can be used to perform all types of strabismus surgery, namely rectus muscle recessions, resections, transpositions, and plications even in the presence of limited motility.
The likelihood that the eyes will stay misaligned over the longer term is higher if the patient is able to achieve some degree of binocular fusion after surgery than if not.
[14] There is also data to suggest that society sees this condition as one that negatively affects many qualities important to self-sufficient function such as responsibility, leadership ability, communication, and even intelligence.
[15] Surgeons take many measures to prevent infection such as careful surgical draping, using povidone iodine as both drops and a solution to soak the sutures in, as well as a post-op course of steroids and antibiotics.
[15] There is generally minimal bleeding during strabismus surgery, but medications such as anti-platelet agents and anticoagulants can lead to vision threatening complications retrobulbar hemorrhage.
[12] Diplopia with normal binocular function is treated with prism glasses, botulinum injections into the muscles, or repeated surgery.
[4] The goal of surgery is to produce a thin line of firm scar tissue where the muscle is reattached to the sclera.
[4] The reflex can also have non cardiac effects such as postoperative nausea and vomiting, which is an extremely common consequence of strabismus surgery in children.