Tacrolimus
[7][8] Tacrolimus inhibits calcineurin, which is involved in the production of interleukin-2, a molecule that promotes the development and proliferation of T cells, as part of the body's learned (or adaptive) immune response.
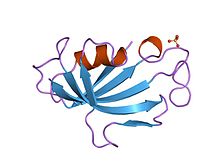
Chemically, it is a macrolide lactone[9] that was first discovered in 1987, from the fermentation broth of a Japanese soil sample that contained the bacterium Streptomyces tsukubensis.
Tacrolimus is normally prescribed as part of a post-transplant cocktail including steroids, mycophenolate, and IL-2 receptor inhibitors such as basiliximab.
[22][23] Contraindications and precautions include:[24] Side effects can be severe and include infection, cardiac damage, hypertension, blurred vision, liver and kidney problems (tacrolimus nephrotoxicity),[26] hyperkalemia, hypomagnesemia, hyperglycemia, diabetes mellitus, itching, lung damage (sirolimus also causes lung damage),[27] and various neuropsychiatric problems such as loss of appetite, insomnia, posterior reversible encephalopathy syndrome, confusion, weakness, depression, vivid nightmares, cramps, neuropathy, seizures, tremors, and catatonia.
[28] In addition, it may potentially increase the severity of existing fungal or infectious conditions such as herpes zoster or polyoma viral infections.
[24] In people receiving immunosuppressants to reduce transplant graft rejection, an increased risk of malignancy (cancer) is a recognised complication.
[30] Tacrolimus and a related drug for eczema (pimecrolimus) were suspected of carrying a cancer risk, though the matter is still a subject of controversy.
The FDA issued a health warning in March 2005 for the drug, based on animal models and a small number of patients.
Until further human studies yield more conclusive results, the FDA recommends that users be advised of the potential risks.
[31] A 2023 systematic review and meta-analysis published in The Lancet Child & Adolescent Health concluded with moderate-certainty evidence that the two drugs were not associated with any increased risk of cancer.
[35] Oral tacrolimus is slowly absorbed in the gastrointestinal tract, with a total bioavailability of 20 to 25% (but with variations from 5 to 67%) and highest blood plasma concentrations (Cmax) reached after one to three hours.
There is evidence to suggest that dosing patients based on rs776746 genotype can result in faster and more frequent achievement of target tacrolimus levels.
[38][39][40][41] Studies have shown that genetic polymorphisms of genes other than CYP3A5, such as NR1I2[42][43] (encoding PXR), also significantly influence the pharmacokinetics of tacrolimus.
The biosynthesis of tacrolimus is hybrid synthesis of both type 1 polyketide synthases (PKS 1) and nonribosomal peptide syntheses (NRPS).
The 19 genes are fkbQ, fkbN, fkbM, fkbD, fkbA, fkbP, fkbO, fkbB, fkbC, fkbL, fkbK, fkbJ, fkbI, fkbH, fkbG, allD, allR, allK and allA.
The biosynthesis of methoxymalonyl CoA to Acyl Carrier protein is proceeded by five enzymes (fkbG, fkbH, fkbI, fkbJ, and fkbK).
[56] The starter unit, DHCHC from the chorismic acid is formed by fkbO enzyme and loaded onto CoA-ligase domain (CoL).
[56][57][58] Tacrolimus has been shown to reduce the risk of serious infections while also increasing remission of kidney function in lupus nephritis.
[59][60] Tacrolimus has been used to suppress the inflammation associated with ulcerative colitis (UC), a form of inflammatory bowel disease.
Although almost exclusively used in trial cases only, tacrolimus has shown to be significantly effective in the suppression of flares of UC.
[61] A 2022 updated Cochrane systematic review found that tacrolimus may be superior to placebo in achieving remission and improvement in UC.