Tetralogy of Fallot
[2] When affected babies cry or have a bowel movement, they may undergo a "tet spell" where they turn cyanotic, have difficulty breathing, become limp, and occasionally lose consciousness.
[18] Other symptoms include a heart murmur which may range from almost imperceptible to very loud, difficulty in feeding, failure to gain weight, retarded growth and physical development, labored breathing (dyspnea) on exertion, clubbing of the fingers and toes, and polycythemia.
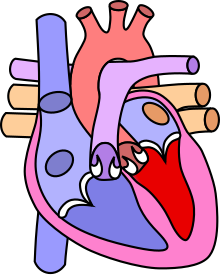
[24] Specific genes associations with TOF include: The Environmental Factors that have been studied to potentially be associated with TOF include: Embryology studies show that anterior malalignment of the aorticopulmonary septum results in the clinical combination of a ventricular septal defect (VSD), pulmonary stenosis, and an overriding aorta.
The right ventricle is dominant prior to birth, receiving 65% of the venous return to the heart, and is the main contributor of blood flow to the lower part of the body, the placenta, and the lungs.
[2] This is not to be confused with the similarly named teratology, a field of medicine concerned with abnormal development and congenital malformations (including tetralogy of Fallot).
[10] Primarily, the degree of right ventricular outflow tract obstruction varies between patients and generally determines clinical symptoms and disease progression.
[51] Natural electrical impulses help maintain blood flowing properly by coordinating contractions in different areas of the heart.
Additionally, close monitoring of the ductus arteriosus is done in the neonatal period to ensure that there is adequate blood flow through the pulmonary valve.
[55] Tet spells may be treated with beta-blockers such as propranolol, but acute episodes require rapid intervention with morphine or intranasal fentanyl[56] to reduce ventilatory drive, a vasopressor such as phenylephrine, or norepinephrine to increase systemic vascular resistance, and IV fluids for volume expansion.
One method to permit pulmonary blood flow post-birth is the stenting of the ductus arterious (DA) through the inducement of a systemic-to-pulmonary shunt.
[59] This open-heart surgery is designed to relieve the right ventricular outflow tract stenosis by careful resection of muscle and to repair the VSD.
[20]: 201–202 However, in symptomatic patients showing worsening blood oxygen levels, severe tet-spells (cyanotic spells), or dependence on prostaglandins from early neonatal period (to keep the ductus arteriosus open) need to be planned fairly urgently[20]: 201–202 Potential surgical repair complications include residual ventricular septal defect, residual outflow tract obstruction, complete atrioventricular block, arrhythmias, aneurysm of right ventricular outflow patch, and pulmonary valve insufficiency.
[59]: 57 This redirected a large portion of the partially oxygenated blood leaving the heart for the body into the lungs, increasing flow through the pulmonary circuit, and relieving symptoms.
[59]: 59 After years of tetralogy of Fallot surgical repair expertise, the attention shifted to the emerging evidence that long-term pulmonary insufficiency is detrimental to right ventricular function and clinical prognosis.
[68][69] As a result, the hunt for surgical procedures to relieve right ventricular outflow tract obstruction while minimizing pulmonary regurgitation has intensified.
[68][69] A constrained right ventricular outflow tract reconstruction with a Dacron patch matched to a nominal pulmonary annulus expansion or an annulus-sparing approach yielded primary complete repair outcomes in 94 TOF infants.
Risk factors for abnormal heart rhythms include: Adult patients with congenital cardiac disease are on the rise at a rate of about 5% per year, outpacing the pediatric population.
[9] Arrhythmia, heart failure, and complications from reoperations are the three primary causes of death in individuals with corrected tetralogy of Fallot.
QRS duration greater than 180 milliseconds, older age at repair (greater than three years), significant pulmonary valve or tricuspid valve regurgitation, history of syncope, multifocal premature ventricular contractions, and ventricular tachycardia are some of the factors associated with sudden death after 30 years of procedure.
Right and left ventricular end-systolic and end-diastolic volume indices, ejection fractions, and the existence of aneurysm generating obstructive outflow are all parameters seen in this research.
[71] Untreated, tetralogy of Fallot rapidly results in progressive right ventricular hypertrophy due to the increased resistance caused by narrowing of the pulmonary trunk.
[61] Patients who have undergone total surgical repair of tetralogy of Fallot have improved hemodynamics and often have good to excellent cardiac function after the operation with some to no exercise intolerance (New York Heart Association Class I-II).
[20]: 205 Cardiovascular and cerebrovascular complications in patients with repaired CHD such as TOF occur earlier in life compared to healthy subjects.
Genetic abnormalities found in TOF may lead to the earlier diagnosis of Danon disease, helping to improve prognostic outcomes.
This patient, who was 16 months old, was initially thought to have asthma, though an autopsy postmortem revealed a cardiac malformation with no ductus arteriosus or ligamentum arteriosum, indicating that the child may have died from TOF.
Fallot initially referred to it as "La maladie bleue", which is French for "the blue disease" or "cyanose cardiaque", translating to "cardiac cyanosis".
[84] The procedure was conducted by surgeon Alfred Blalock and cardiologist Helen B. Taussig, with Vivien Thomas also providing substantial contributions and listed as an assistant.
[87][12] Symptoms of these diseases include an unusually high rate of breathing (tachypnea), a blue hue to the skin (cyanosis), wheezing, a rapid heartbeat (tachycardia), and/or an abnormally enlarged liver, which are similar to those of other congenital heart problems (hepatomegaly).
[12] Congenital Mitral valve stenosis symptoms include a wide array such as respiratory infections, breathing difficulties, heart palpitations and coughing.
[12] Acquired mitral valve stenosis symptoms also include a wide array such as consciousness losses, angina, general weakness and abdominal discomfort.