Ulcerative colitis
[1] Several medications are used to treat symptoms and bring about and maintain remission, including aminosalicylates such as mesalazine or sulfasalazine, steroids, immunosuppressants such as azathioprine, and biologic therapy.
[12] With proctitis (inflammation of the rectum), people with UC may experience urgency or rectal tenesmus, which is the urgent desire to evacuate the bowels but with the passage of little stool.
Indicators of low risk for future complications in mild and moderate UC include the following parameters: exhibiting less than 6 stools daily and lack of fever/weight loss.
Other indicators include lack of extraintestinal symptoms, low levels of the inflammatory markers C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR), and fecal calprotectin, and later age of diagnosis (over 40 years).
[19] Mild disease lacks systemic signs of toxicity (e.g. fever, chills, weight changes) and exhibits normal levels of the serum inflammatory markers ESR and CRP.
[32] Inflammation may also involve the white part of the eye (sclera) or the overlying connective tissue (episclera), causing conditions called scleritis and episcleritis.
This condition represents a chronic process in which follicles become occluded leading to recurring inflammation of nodules and abscesses and even fistulas tunnels in the skin that drain fluid.
[18] Ulcerative colitis (UC) has a significant association with primary sclerosing cholangitis (PSC), a progressive inflammatory disorder of small and large bile ducts.
[12] Twelve regions of the genome may be linked to UC, including, in the order of their discovery, chromosomes 16, 12, 6, 14, 5, 19, 1, and 3,[46] but none of these loci has been consistently shown to be at fault, suggesting that the disorder is influenced by multiple genes.
[46] Multiple autoimmune disorders are associated with ulcerative colitis, including celiac disease,[48] psoriasis,[49] lupus erythematosus,[50] rheumatoid arthritis,[51] episcleritis, and scleritis.
[66] An increased amount of colonic sulfate-reducing bacteria has been observed in some people with ulcerative colitis, resulting in higher concentrations of the toxic gas hydrogen sulfide.
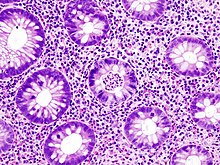
[13] The initial diagnostic workup for ulcerative colitis consists of a complete history and physical examination, assessment of signs and symptoms, laboratory tests and endoscopy.
In circumstances of severe UC, radiographic findings may include thickening of the mucosa, often termed "thumbprinting", which indicates swelling due to fluid displacement (edema).
It is important to note that barium enema should not be conducted in patients exhibiting very severe symptoms as this may slow or stop stool passage through the colon causing ileus and toxic megacolon.
Adding corticosteroids such as prednisone is also common in active disease, especially if remission is not achieved through mesalazine monotherapy,[96][97] but they are not used in long-term treatment as their risks then outweigh their benefits.
Immunosuppressive medications such as azathioprine and biological agents such as infliximab, adalimumab, ustekinumab, vedolizumab, or risankizumab are given in severe disease or if a patient cannot achieve remission with mesalazine and corticosteroids.
[102][103] In 2018, tofacitinib was approved for treatment of moderately to severely active ulcerative colitis in the United States, the first oral medication indicated for long term use in this condition.
[111] Many 5-ASA drugs have been developed with the aim of delivering the active compound to the large intestine to maintain therapeutic efficacy but with reduction of the side effects associated with the sulfapyridine moiety in sulfasalazine.
[112][113] Rectal suppository, foam or liquid enema formulations of 5-ASA are used for colitis affecting the rectum, sigmoid or descending colon, and have been shown to be effective especially when combined with oral treatment.
[124] In one double-blind, placebo-controlled study conducted in the United Kingdom, 48.6% of people with UC who used the nicotine patch, in conjunction with their standard treatment, showed complete resolution of symptoms.
[129][131] Anticholinergic drugs, more specifically muscarinic antagonists, are sometimes used to treat abdominal cramps in connection with ulcerative colitis through their calming effect on colonic peristalsis (reducing both amplitude and frequency) and intestinal tone.
[142][143] Unlike in Crohn's disease, the gastrointestinal aspects of ulcerative colitis can generally be cured by surgical removal of the large intestine, though extraintestinal symptoms may persist.
[14] The removal of the entire large intestine, known as a proctocolectomy, results in a permanent ileostomy – where a stoma is created by pulling the terminal ileum through the abdomen.
This involves removing the large majority of the remaining rectal stump and creating a new "rectum" by fashioning the end of the small intestine into a pouch and attaching it to the anus.
Curcumin (turmeric) therapy, in conjunction with taking the medications mesalamine or sulfasalazine, may be effective and safe for maintaining remission in people with quiescent ulcerative colitis.
[177] As with Crohn's disease, the rates of UC are greater among Ashkenazi Jews and decreases progressively in other persons of Jewish descent, non-Jewish Caucasians, Africans, Hispanics, and Asians.
[189] Helminthic therapy using the whipworm Trichuris suis has been shown in a randomized control trial from Iowa to show benefit in people with ulcerative colitis.
Both helminthic therapy and fecal microbiota transplant induce a characteristic Th2 white cell response in the diseased areas, which was unexpected given that ulcerative colitis was thought to involve Th2 overproduction.
[190] Alicaforsen is a first generation antisense oligodeoxynucleotide designed to bind specifically to the human ICAM-1 messenger RNA through Watson-Crick base pair interactions in order to subdue expression of ICAM-1.
[191] Increased expression of ICAM-1 has been observed within the inflamed intestinal mucosa of ulcerative colitis patients, where ICAM-1 over production correlated with disease activity.