Bipolar disorder
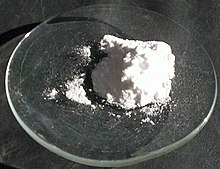
[16] Mood stabilizers, particularly lithium, and certain anticonvulsants, such as lamotrigine and valproate, as well as atypical antipsychotics, including quetiapine, olanzapine, and aripiprazole are the mainstay of long-term pharmacologic relapse prevention.
[24] Interest in functioning in the assessment of patients with bipolar disorder is growing, with an emphasis on specific domains such as work, education, social life, family, and cognition.
[26] Due to lifestyle choices and the side effects of medications, the risk of death from natural causes such as coronary heart disease in people with bipolar disorder is twice that of the general population.
[24] Since a diagnosis of bipolar disorder requires a manic or hypomanic episode, many affected individuals are initially misdiagnosed as having major depression and treated with prescribed antidepressants.
[57][60] The largest and most recent genome-wide association study failed to find any locus that exerts a large effect, reinforcing the idea that no single gene is responsible for bipolar disorder in most cases.
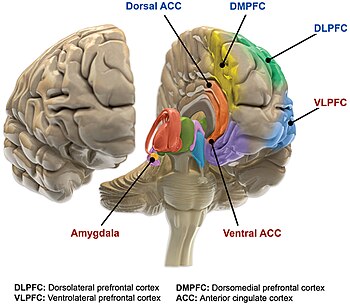
There is evidence supporting an association between early-life stress and dysfunction of the hypothalamic-pituitary-adrenal axis leading to its overactivation, which may play a role in the pathogenesis of bipolar disorder.
Increased dopaminergic activity has been hypothesized in manic states due to the ability of dopamine agonists to stimulate mania in people with bipolar disorder.
[5][96] Its diagnosis is based on the self-reported experiences of the individual, abnormal behavior reported by family members, friends or co-workers, observable signs of illness as assessed by a clinician, and ideally a medical work-up to rule out other causes.
[109] Bipolar II disorder was established as a diagnosis in 1994 within DSM IV; though debate continues over whether it is a distinct entity, part of a spectrum, or exists at all.
Individuals who have subthreshold symptoms that cause clinically significant distress or impairment, but do not meet full criteria for one of the three subtypes may be diagnosed with other specified or unspecified bipolar disorder.
Other specified bipolar disorder is used when a clinician chooses to explain why the full criteria were not met (e.g., hypomania without a prior major depressive episode).
[33] The definition of rapid cycling most frequently cited in the literature (including the DSM-V and ICD-11) is that of Dunner and Fieve: at least four major depressive, manic, hypomanic or mixed episodes during a 12-month period.
[41][46][57][121] A thorough longitudinal analysis of symptoms and episodes, assisted if possible by discussions with friends and family members, is crucial to establishing a treatment plan where these comorbidities exist.
Depressive episodes more commonly present with sleep disturbance, fatigue, hopelessness about the future, slowed thinking, and poor concentration and memory; the last three symptoms are seen in what is known as pseudodementia.
[133] Longitudinal studies have indicated that full-blown manic stages are often preceded by a variety of prodromal clinical features, providing support for the occurrence of an at-risk state of the disorder when an early intervention might prevent its further development and/or improve its outcome.
[138][139][140] Psychotherapy aims to assist a person with bipolar disorder in accepting and understanding their diagnosis, coping with various types of stress, improving their interpersonal relationships, and recognizing prodromal symptoms before full-blown recurrence.
Valproate and carbamazepine are teratogenic and should be avoided as a treatment in women of childbearing age, but discontinuation of these medications during pregnancy is associated with a high risk of relapse.
[158] Electroconvulsive therapy (ECT) is an effective form of treatment for acute mood disturbances in those with bipolar disorder, especially when psychotic or catatonic features are displayed.
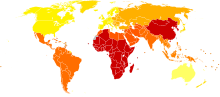
[166] A lifelong condition with periods of partial or full recovery in between recurrent episodes of relapse,[46][168] bipolar disorder is considered to be a major health problem worldwide because of the increased rates of disability and premature mortality.
[4][47] When compared to the general population, people with bipolar disorder also have higher rates of other serious medical comorbidities including diabetes mellitus, respiratory diseases, HIV, and hepatitis C virus infection.
[5][180] However, the course of illness (duration, age of onset, number of hospitalizations, and the presence or not of rapid cycling) and cognitive performance are the best predictors of employment outcomes in individuals with bipolar disorder, followed by symptoms of depression and years of education.
[180] A naturalistic study in 2003 by Tohen and coworkers from the first admission for mania or mixed episode (representing the hospitalized and therefore most severe cases) found that 50% achieved syndromal recovery (no longer meeting criteria for the diagnosis) within six weeks and 98% within two years.
Including sub-threshold diagnostic criteria, such as one or two symptoms over a short time-period, an additional 5.1% of the population, adding up to a total of 6.4%, were classified as having a bipolar spectrum disorder.
The subtypes bipolar II and rapid cycling have been included since the DSM-IV, based on work from the 1970s by David Dunner, Elliot Gershon, Frederick Goodwin, Ronald Fieve, and Joseph Fleiss.
Braunstein was diagnosed with bipolar disorder in 1985 and his concerts with the ME/2 Orchestra were conceived in order to create a welcoming performance environment for his musical colleagues, while also raising public awareness about mental illness.
Kay Redfield Jamison, a clinical psychologist and professor of psychiatry at the Johns Hopkins University School of Medicine, profiled her own bipolar disorder in her memoir An Unquiet Mind (1995).
[217] Several celebrities have also publicly shared that they have bipolar disorder; in addition to Carrie Fisher and Stephen Fry these include Catherine Zeta-Jones, Mariah Carey, Kanye West,[218] Jane Pauley, Demi Lovato,[211] Selena Gomez,[219] and Russell Brand.
In Mr. Jones (1993), (Richard Gere) swings from a manic episode into a depressive phase and back again, spending time in a psychiatric hospital and displaying many of the features of the syndrome.
[221] In The Mosquito Coast (1986), Allie Fox (Harrison Ford) displays some features including recklessness, grandiosity, increased goal-directed activity and mood lability, as well as some paranoia.
[126] Some treatment research suggests that psychosocial interventions that involve the family, psychoeducation, and skills building (through therapies such as CBT, DBT, and IPSRT) can benefit in addition to pharmacotherapy.