Vocal cord dysfunction
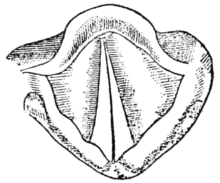
[1] It is characterized by abnormal closure of the vocal folds, which can result in significant difficulties and distress during breathing, particularly during inhalation.
[3] Treatment of VCD often combines behavioral, medical, and psychological approaches, most often including an otolaryngologist, a psychologist, and a speech-language pathologist.
[4] They may report tightness in the throat or chest, choking, stridor on inhalation and wheezing, which can resemble the symptoms of asthma.
[5] Many of the symptoms are not specific to vocal cord dysfunction and can resemble a number of conditions that affect the upper and lower airways.
[11] Published studies emphasize anxiety or stress as a primary cause while more recent literature indicates a likely physical etiology.
[4] Experiencing or witnessing a traumatic event related to breathing (such as a near-drowning or life-threatening asthma attack, for example), has also been identified as a risk factor for VCD.
[10] VCD has also been associated with certain neurologic diseases including Arnold-Chiari malformation, cerebral aqueduct stenosis, cortical or upper motor neuron injury (such as that resulting from stroke), amyotrophic lateral sclerosis (ALS), parkinsonism syndromes and other movement disorders.
[10] Physical exercise (including, but not limited to, competitive athletics) is one of the major triggers for VCD episodes, leading to its frequent misdiagnosis as exercise-induced asthma.
[10][5][6] Other triggers include airborne pollutants and irritants such as smoke, dust, gases, soldering fumes, cleaning chemicals such as ammonia, perfumes, and other odors.
[5][4] Gastroesophageal reflux disease (GERD) and rhinosinusitis (inflammation of the paranasal sinuses and nasal cavity) may also play a role in inflaming the airway and leading to symptoms of VCD as discussed below.
[10][4] Two major causes of laryngeal inflammation and hyperresponsiveness are gastroesophageal reflux disease (GERD) and postnasal drip (associated with rhinosinusitis, allergic or nonallergic rhinitis, or a viral upper respiratory tract infection (URI)).
[5][6] Other causes of laryngeal hyperresponsiveness include inhalation of toxins and irritants, cold and dry air, episodic croup and laryngopharyngeal reflux (LPR).
[6] The following increases an individual's chances for acquiring VCD:[13] The most effective diagnostic strategy is to perform laryngoscopy during an episode, at which time abnormal movement of the cords, if present, can be observed.
In individuals who experience a persistent difficulty with inhaling, consideration should be given to a neurological cause such as brain stem compression, cerebral palsy, etc.
[1] Intervention goals target teaching a client breathing and relaxation exercises so that they can control their throat muscles and keep the airway open, allowing air to flow in and out.
[4] Breathing techniques can be taught to reduce tension in the throat, neck, and upper body and bring attention to the flow of air during respiration.
[4] Other techniques can involve breathing through a straw and panting, which widens the opening of the throat by activating the Posterior cricoarytenoid (PCA) muscle.
[4][19] Endoscopic feedback can also be used to show a patient what is happening when they are doing simple tasks such as taking a deep breath or speaking on an inspiration.
Managing GERD has also been found to relieve laryngospasm, a spasm of the vocal cords that makes breathing and speaking difficult.
[4][21][22] Psychological interventions including psychotherapy, cognitive behavioral therapy (CBT), Biofeedback, and teaching self-hypnosis are also suggested to treat VCD.
The aim of Biofeedback is to educate the client on what happens to the vocal cords during breathing and to help them learn to control their symptoms.
[4] Choosing an intervention strategy needs to be assessed by a multidisciplinary team and individualized therapy planned carefully, keeping the characteristics of each patient in mind.
[7] Additionally, there is currently no research that has studied whether the underlying cause of VCD makes a difference in the resolution of symptoms or in the long-term prognosis of the impairment.
[5] Most studies agree that symptoms of VCD improve in patients and few continue to require asthma medications six months post speech therapy intervention.
[6][25] Meanwhile, much higher VCD incidence rates have also been reported in asthmatic populations, ranging from 14% in children with refractory asthma to 40% in adults with the same complaint.