Paracetamol
[33] Short term adverse effects are uncommon and similar to ibuprofen,[34] but paracetamol is typically safer than nonsteroidal anti-inflammatory drugs (NSAIDs) for long-term use.
[36][37] Chronic consumption of paracetamol may result in a drop in hemoglobin level, indicating possible gastrointestinal bleeding,[38] and abnormal liver function tests.
[15][27] American College of Rheumatology and Arthritis Foundation guideline for the management of osteoarthritis notes that the effect size in clinical trials of paracetamol has been very small, which suggests that for most individuals it is ineffective.
[62] Similarly, the ESCEO algorithm for the treatment of knee osteoarthritis recommends limiting the use of paracetamol to short-term rescue analgesia only.
[30][27][29] Paracetamol is effective for acute migraine:[16] 39 % of people experience pain relief at one hour compared with 20 % in the control group.
[25] Full therapeutic doses of nonsteroidal anti-inflammatory drugs (NSAIDs) ibuprofen, naproxen or diclofenac are clearly more efficacious than the paracetamol/codeine combination which is frequently prescribed for dental pain.
[80] After 13 weeks of paracetamol therapy for knee pain, a drop in hemoglobin level indicating gastrointestinal bleeding was observed in 20 % of participants, this rate being similar to the ibuprofen group.
[37] A 2022 double-blind, placebo-controlled, crossover study has provided evidence that daily, high-dose use (4 g per day) of paracetamol increases systolic BP.
[85] However, the most recent research suggests that there is no association,[86] and that the frequency of asthma exacerbations in children after paracetamol is the same as after another frequently used pain killer, ibuprofen.
However, indications exist of a possible increase in the risk of asthma and developmental and reproductive disorders in the offspring of women with prolonged use of paracetamol during pregnancy.
[82][98][99] There is also an argument that the large number, consistency, and robust designs of the studies provide strong evidence in favor of paracetamol causing the increased risk of these neurodevelopmental disorders.
[82] The consensus recommendation appears to be to avoid prolonged use of paracetamol in pregnancy and use it only when necessary, at the lowest effective dosage, and for the shortest time.
[39] While a majority of adult overdoses are linked to suicide attempts, many cases are accidental, often due to the use of more than one paracetamol-containing product over an extended period.
[109] According to the FDA, in the United States, "56,000 emergency room visits, 26,000 hospitalizations, and 458 deaths per year [were] related to acetaminophen-associated overdoses during the 1990s.
The first symptoms of overdose usually begin several hours after ingestion, with nausea, vomiting, sweating, and pain as acute liver failure starts.
[120] Out of the inducers studied, the evidence of potentially increased liver toxicity in paracetamol overdose exists for phenobarbital, primidone, isoniazid, and possibly St John's wort.
[125] Supporting the first mechanism, pharmacologically and in its side effects, paracetamol is close to classical nonsteroidal anti-inflammatory drugs (NSAIDs) that act by inhibiting COX-1 and COX-2 enzymes and especially similar to selective COX-2 inhibitors.
[125][126] The anti-inflammatory action of paracetamol (via COX inhibition) has also been found to primarily target the central nervous system and not peripheral areas of the body, explaining the lack of side effects associated with conventional NSAIDs such as gastric bleeding.
Even in the fasting state, the rate of absorption of paracetamol is variable and depends on the formulation, with maximum plasma concentration being reached after 20 minutes to 1.5 hours.
[6] Its plasma terminal elimination half-life is 1.9–2.5 hours,[6] and volume of distribution is roughly 50 L.[132] Protein binding is negligible, except under the conditions of overdose, when it may reach 15–21 %.
[134] A minor metabolic pathway (5–15 %) of oxidation by cytochrome P450 enzymes, mainly by CYP2E1, forms a toxic metabolite known as NAPQI (N-acetyl-p-benzoquinone imine).
p-Aminophenol is then converted in the brain by fatty acid amide hydrolase into AM404, a compound that may be partially responsible for the analgesic action of paracetamol.
[139] Acetanilide was the first aniline derivative serendipitously found to possess analgesic as well as antipyretic properties, and was quickly introduced into medical practice under the name of Antifebrin by Cahn & Hepp in 1886.
[141] Some reports state that Cahn & Hepp or a French chemist called Charles Gerhardt first synthesized paracetamol in 1852.
[145] Von Mering's claims remained essentially unchallenged for half a century until two teams of researchers from the United States analyzed the metabolism of acetanilide and phenacetin.
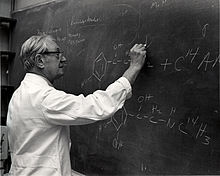
[146] In 1948, Bernard Brodie, Julius Axelrod and Frederick Flinn confirmed that paracetamol was the major metabolite of acetanilide in humans, and established that it was just as efficacious an analgesic as its precursor.
[151] In the United Kingdom, marketing of paracetamol began in 1956 by Sterling-Winthrop Co. as Panadol, available only by prescription, and promoted as preferable to aspirin since it was safe for children and people with ulcers.
[156] In June 2009, an FDA advisory committee recommended that new restrictions be placed on paracetamol use in the United States to help protect people from the potential toxic effects.
Committee members were particularly concerned by the fact that the then-present maximum dosages of paracetamol had been shown to produce alterations in liver function.
[157] In January 2011, the FDA asked manufacturers of prescription combination products containing paracetamol to limit its amount to no more than 325 mg per tablet or capsule and began requiring manufacturers to update the labels of all prescription combination paracetamol products to warn of the potential risk of severe liver damage.