Aspergillosis
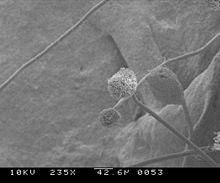
Aspergillosis is a fungal infection of usually the lungs,[2] caused by the genus Aspergillus, a common mould that is breathed in frequently from the air, but does not usually affect most people.
[3][4] It generally occurs in people with lung diseases such as asthma, cystic fibrosis or tuberculosis, or those who are immunocompromised such as those who have had a stem cell or organ transplant or those who take medications such as steroids and some cancer treatments which suppress the immune system.
Most cases of acute aspergillosis occur in people with severely compromised immune systems such as those undergoing bone marrow transplantation.
Most people are thought to inhale thousands of Aspergillus spores daily but without effect due to an efficient immune response.
[2] A rapidly invasive Aspergillus infection in the lungs often causes cough, fever, chest pain, and difficulty breathing.
[18] Aspergillosis is caused by Aspergillus, a common mold, which tends to affect people who already have a lung disease such as cystic fibrosis or asthma, or who cannot fight infection themselves.
[19] People who are immunocompromised — such as patients undergoing hematopoietic stem cell transplantation, chemotherapy for leukaemia, or AIDS — are at an increased risk for invasive aspergillosis infections.
If the underlying neutropenia is not fixed, rapid and uncontrolled hyphal growth of the invasive fungi will occur and result in negative health outcomes.
[20] In addition to decreased neutrophil degranulation, the antiviral response against Flu and SARS-CoV-2 viruses, mediated by type I and type II interferon, is diminished jointly with the local antifungal immune response measured in the lungs of patients with IAPA (Influenza-Associated Pulmonary Aspergillosis) and CAPA (COVID-19-Associated Pulmonary Aspergillosis).
However, in those with underlying lung diseases, such as cystic fibrosis or bronchiectasis, this mucociliary clearance mechanism is impaired and aspergillus spores (which are 2-5 μm in diameter) are able to colonize the airways and sinuses.
[13] False-positive Aspergillus galactomannan tests have been found in patients on intravenous treatment with some antibiotics or fluids containing gluconate or citric acid such as some transfusion platelets, parenteral nutrition, or PlasmaLyte.
[29] A systematic review has evaluated the diagnostic accuracy of polymerase chain reaction (PCR) tests in people with defective immune systems from medical treatment such as chemotherapy.
[30] Evidence suggests PCR tests have moderate diagnostic accuracy when used for screening for invasive aspergillosis in high risk groups.
[31][32][33] The current medical treatments for aggressive invasive aspergillosis include voriconazole and liposomal amphotericin B in combination with surgical debridement.
Captive raptors, such as falcons and hawks, are susceptible to this disease if they are kept in poor conditions and especially if they are fed pigeons, which are often carriers of "asper".
It can also spread to the rest of the body; this is termed disseminated aspergillosis and is rare, usually affecting individuals with underlying immune disorders.
[citation needed] In 2019, an outbreak of aspergillosis struck the rare kākāpō, a large flightless parrot endemic to New Zealand.