Atrial septal defect
A layer of tissue called the septum primum acts as a valve over the foramen ovale during fetal development.
After birth, the pressure in the right side of the heart drops as the lungs open and begin working, causing the foramen ovale to close entirely.
The six types of atrial septal defects are differentiated from each other by whether they involve other structures of the heart and how they are formed during the developmental process during early fetal development.
[citation needed] Complications of an uncorrected secundum ASD include pulmonary hypertension, right-sided congestive heart failure[7].
[citation needed] PFO is linked to stroke, sleep apnea, migraine with aura, cluster headache, decompression sickness, Raynaud's phenomenon, hyperventilation syndrome, transient global amnesia (TGA), and leftsided carcinoid heart disease (mitral valve).
PFO is common in patients with an atrial septal aneurysm (ASA), a much rarer condition, which is also linked to cryptogenic (i.e., of unknown cause) stroke.
[citation needed] A sinus venosus ASD that involves the superior vena cava makes up 2 to 3% of all interatrial communication.
[22] Common (or single) atrium is a failure of development of the embryologic components that contribute to the atrial septal complex.
Patients with an uncorrected atrial septal defect may be at increased risk for developing a cardiac arrhythmia, as well as more frequent respiratory infections.
[20] ASDs, and particularly PFOs, are a predisposing venous blood carrying inert gases, such as helium or nitrogen does not pass through the lungs.
In an individual with ASD, these emboli can potentially enter the arterial system, which can cause any phenomenon attributed to acute loss of blood to a portion of the body, including cerebrovascular accident (stroke), infarction of the spleen or intestines, or even a distal extremity (i.e., finger or toe).
Most individuals with a significant ASD are diagnosed in utero or in early childhood with the use of ultrasonography or auscultation of the heart sounds during physical examination.
[citation needed] Adults with an uncorrected ASD present with symptoms of dyspnea on exertion (shortness of breath with minimal exercise), congestive heart failure, or cerebrovascular accident (stroke).
[36] The physical findings in an adult with an ASD include those related directly to the intracardiac shunt and those that are secondary to the right heart failure that may be present in these individuals.
The increased blood volume in the right ventricle causes the pulmonic valve to stay open longer during ventricular systole.
Because the atria are linked via the atrial septal defect, inspiration produces no net pressure change between them, and has no effect on the splitting of S2.
[citation needed] If agitated saline is injected into a peripheral vein during echocardiography, small air bubbles can be seen on echocardiographic imaging.
Newer techniques to visualize these defects involve intracardiac imaging with special catheters typically placed in the venous system and advanced to the level of the heart.
[citation needed] A less invasive method for detecting a PFO or other ASDs than transesophagal ultrasound is transcranial Doppler with bubble contrast.
[citation needed] A common finding in the ECG is the presence of incomplete right bundle branch block, which is so characteristic that if it is absent, the diagnosis of ASD should be reconsidered.
Previous studies did not identify a clear benefit of PFO closure over antiplatelet therapy in reducing recurrent ischemic stroke.
[47][48] Based on the most up to date evidence, PFO closure is more effective at reducing recurrent ischemic stroke when compared to medical therapy.
A recent review of the literature supports this hypothesis recommending anticoagulation over the use of antiplatelet therapy in patients with PFO and cryptogenic stroke.
Individuals with a pulmonary vascular resistance (PVR) less than 7 wood units show regression of symptoms (including NYHA functional class).
(If Eisenmenger's physiology has set in, the right-to-left shunt must be shown to be reversible with pulmonary artery vasodilators prior to surgery.
)[citation needed] Surgical mortality due to closure of an ASD is lowest when the procedure is performed prior to the development of significant pulmonary hypertension.
[citation needed] Surgical closure of an ASD involves opening up at least one atrium and closing the defect with a patch under direct visualization.
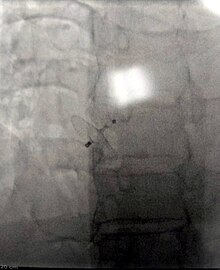
[citation needed] Percutaneous device closure involves the passage of a catheter into the heart through the femoral vein guided by fluoroscopy and echocardiography.
The ASO consists of two self-expandable round discs connected to each other with a 4-mm waist, made up of 0.004– to 0.005-inch Nitinol wire mesh filled with Dacron fabric.
[55] Studies evaluating percutaneous ASD closure among pediatric and adult population show that this is relatively safer procedure and has better outcomes with increasing hospital volume.

HV : right ventricle; VCS : superior vena cava; VCI : inferior vena cava
1 : upper sinus venosus defect ; 2 : lower sinus venosus defect ; 3 : secundum defect; 4 : defect involving coronary sinus ; 5 ; primum defect .