Bladder cancer
[1] Women with bladder cancer and haematuria are often misdiagnosed with urinary tract infections, delaying appropriate diagnosis and treatment.
The gold standard is cystoscopy, wherein a flexible camera is threaded through the urethra and into the bladder to visually inspect for cancerous tissue.
The dye fluoresces when the cystoscope shines blue light on it, allowing for more accurate detection of small tumors.
This is typically done by injecting a dye into the blood that the kidneys will filter into the urinary tract, then imaging by CT scanning.
[12] The remaining cases are sarcomas (from the bladder muscle) or small-cell cancer (from neuroendocrine cells), both of which are relatively rare.
[4] NMIBC is primarily treated by surgically removing all tumors by TURBT in the same procedure used to collect biopsy tissue for diagnosis.
[15][18] Tumors that do not respond to BCG may be treated with the alternative immune stimulants nadofaragene firadenovec (sold as "Adstiladrin", a gene therapy that makes bladder cells produce an immunostimulant protein), nogapendekin alfa inbakicept ("Anktiva", a combination of immunostimulant proteins), or pembrolizumab ("Keytruda", an immune checkpoint inhibitor).
[19] People whose tumors continue to grow are often treated with surgery to remove the bladder and surrounding organs, called radical cystectomy.
[20] The bladder, several adjacent lymph nodes, the lower ureters, and nearby internal genital organs – in men the prostate and seminal vesicles; in women the womb and part of the vaginal wall – are all removed.
The most common method is by ileal conduit, where a piece of the ileum (part of the small intestine) is removed and used to transport urine from the ureters to a new surgical opening (stoma) in the abdomen.
The affected person empties the new urine reservoir several times each day by self-catheterization – passing a narrow tube through the stoma.
[23] Those with no CIS or urinary blockage may undergo TURBT to remove visible tumors, followed by chemotherapy and radiotherapy, known as "trimodality therapy".
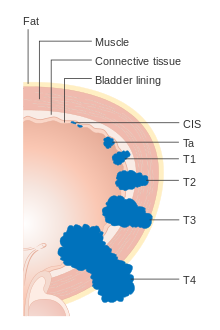
[23] Stage IV bladder cancer that has reached the pelvic or abdominal wall (T4b), spread to distant lymph nodes (M1a) or other parts of the body (M1b) is difficult to completely remove surgically, the initial treatment usually being chemotherapy.
[27] The 2022 standard of care for metastatic bladder cancer is combination treatment with the chemotherapy drugs cisplatin and gemcitabine.
[30] Those whose disease responds to chemotherapy benefit from switching to immune checkpoint inhibitors pembrolizumab or atezolizumab ("Tecentriq") for long-term maintenance therapy.
[32][34] Those with genetic alterations that activate the proteins FGFR2 or FGFR3 (around 20% of those with metastatic bladder cancer) can also benefit from the FGFR inhibitor erdafitinib ("Balversa").
Vinflunine is used in Europe, while paclitaxel, docetaxel, and pemetrexed are used in the United States; only a minority of those treated improve on these therapies.
It is common for those recovering from surgery to experience gastrointestinal problems (29% of those who underwent radical cystectomy), infections (25%), and other issues with the surgical wound (15%).
[37] Checkpoint inhibitor (immunotherapy) side effects commonly include injection site pain, soreness, itchiness or rash.
Additional flu-like symptoms may occur like fever, weakness, dizziness, nausea or vomiting, headache, fatigue, or blood pressure changes.
Autoimmune reactions are possible because checkpoint inhibitors function by altering or removing immune system safeguards which can cause serious or even life-threatening problems.
Very rarely, a hole might form through the wall of the esophagus, stomach, small intestine, large bowel, rectum, or gallbladder.
[40] Radiotherapy acute side effects involve the gastrointestinal system, e.g., diarrhea and constipation; the urinary tract; and may cause cervicitis.
Common late effects include: premature ovarian failure; telangiectasias, and subsequent hemorrhage; and progressive myelopathy.
[43] Radiation also induces secondary malignancies such as leukemia, lymphoma, bone and soft-tissue sarcoma with occurrence rates between 0.2-1.0% per year for each.
[55] Worms can be cleared by treatment with praziquantel, which reduces bladder cancer cases in schistosomiasis endemic areas.
Most of these are variants in genes involved in metabolism of carcinogens (NAT2, GSTM1, and UGT1A6), controlling cell growth (TP63, CCNE1, MYC, and FGFR3), or repairing DNA damage (NBN, XRCC1 and 3, and ERCC2, 4, and 5).
They also considered available data on exercise, body fat, and consumption of dairy, red meat, fish, grains, legumes, eggs, fats, soft drinks, alcohol, juices, caffeine, sweeteners, and various vitamins and minerals; for each they found insufficient data to link the lifestyle factor to bladder cancer risk.
Parts of the urothelium can accumulate DNA mutations over years, making these areas more likely to give rise to tumors.
Those whose tumors have spread to nearby lymph nodes (stage 3 disease) have worse prognoses; 36% survive at least five years from diagnosis.