Renal cell carcinoma
[10] Today, renal cell carcinoma (RCC) is often asymptomatic, meaning it presents no symptoms, and is commonly detected incidentally during examinations for unrelated medical conditions.
[11] Other signs and symptom may include haematuria;[10] loin pain;[10] abdominal mass;[12] malaise, which is a general feeling of unwellness;[12] weight loss and/or loss of appetite;[13] anaemia resulting from depression of erythropoietin;[10] erythrocytosis (increased production of red blood cells) due to increased erythropoietin secretion;[10] varicocele, which is seen in males as an enlargement of the pampiniform plexus of veins draining the testis (more often the left testis)[12] hypertension (high blood pressure) resulting from secretion of renin by the tumour;[14] hypercalcemia, which is elevation of calcium levels in the blood;[15] sleep disturbance or night sweats;[13] recurrent fevers;[13] and chronic fatigue.
[16] The greatest risk factors for RCC are lifestyle-related: smoking, obesity and hypertension (high blood pressure) have been estimated to account for up to 50% of cases.
[17] Occupational exposure to some chemicals such as asbestos, cadmium, lead, chlorinated solvents, petrochemicals and PAH (polycyclic aromatic hydrocarbon) has been examined by multiple studies with inconclusive results.
[23] Hereditary factors have a minor impact on individual susceptibility with immediate relatives of people with RCC having a two to fourfold increased risk of developing the condition.
[28] Although this disease lacks characterization in the early stages of tumor development, considerations based on diverse clinical manifestations, as well as resistance to radiation and chemotherapy are important.
The main diagnostic tools for detecting renal cell carcinoma are ultrasound, computed tomography (CT) scanning and magnetic resonance imaging (MRI) of the kidneys.
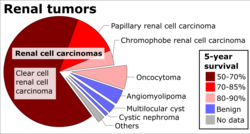
Since the publication of the latest iteration of the WHO classification in 2004, several novel renal tumour subtypes have been described:[38] Laboratory tests are generally conducted when the patient presents with signs and symptoms that may be characteristic of kidney impairment.
They are not primarily used to diagnose kidney cancer, due to its asymptomatic nature and are generally found incidentally during tests for other illnesses such as gallbladder disease.
[45] However, the advances of diagnostic modalities are able to incidentally diagnose a great proportion of patients with renal lesions that may appear to be small in size and of benign state.
[47] The Bosniak classification system for cystic renal lesions classifies them into groups that are benign and those that need surgical resection, based on specific imaging features.
[citation needed] Contrast-enhanced computed tomography (CT) scanning is routinely used to determine the stage of the renal cell carcinoma in the abdominal and pelvic regions.
[51] Ultrasonographic examination can be useful in evaluating questionable asymptomatic kidney tumours and cystic renal lesions if computed tomography imaging is inconclusive.
This safe and non-invasive radiologic procedure uses high frequency sound waves to generate an interior image of the body on a computer monitor.
The image generated by the ultrasound can help diagnose renal cell carcinoma based on the differences of sound reflections on the surface of organs and the abnormal tissue masses.
However this is not routinely performed because when the typical imaging features of renal cell carcinoma are present, the possibility of an incorrectly negative result together with the risk of a medical complication to the patient may make it unfavourable from a risk-benefit perspective.
Patients on dialysis or those who have renal insufficiency should avoid this contrasting material as it may induce a rare, yet severe, side effect known as nephrogenic systemic fibrosis.
MRI scans should also be considered to evaluate tumour extension which has grown in major blood vessels, including the vena cava, in the abdomen.
Gross examination often shows a yellowish, multilobulated tumor in the renal cortex, which frequently contains zones of necrosis, haemorrhage and scarring.
Sarcomatoid changes (morphology and patterns of IHC that mimic sarcoma, spindle cells) can be observed within any RCC subtype and are associated with more aggressive clinical course and worse prognosis.
[63] The recommended histologic grading schema for RCC is the Fuhrman system (1982), which is an assessment based on the microscopic morphology of a neoplasm with haematoxylin and eosin (H&E staining).
Active surveillance or "watchful waiting" is becoming more common as small renal masses or tumours are being detected and also within the older generation when surgery is not always suitable.
[69] Active surveillance involves completing various diagnostic procedures, tests and imaging to monitor the progression of the RCC before embarking on a more high risk treatment option like surgery.
[10] The partial nephrectomy involves the removal of the affected tissue only, sparing the rest of the kidney, Gerota's fascia and the regional lymph nodes.
[4] For small exophytic lesions that do not extensively involve the major vessels or urinary collecting system, a partial nephrectomy (also referred to as "nephron sparing surgery") can be performed.
[97] More medications are expected to become available in the near future as several clinical trials are currently being conducted for new targeted treatments,[98] including: atezolizumab, varlilumab, durvalumab, avelumab, LAG525, MBG453, TRC105, and savolitinib.
[104] The prognosis is influenced by several factors, including tumour size, degree of invasion and metastasis, histologic type, and nuclear grade.
For instance, younger people (among 20–40 years old) have a better outcome despite having more symptoms at presentation, possibly due to lower rates spread of cancer to the lymph nodes (stage III).
[117] He described the case of Françoise Levelly, a 35-year-old woman, who presented to Brest Civic Hospital on April 6, 1809, supposedly in the late stages of pregnancy.
In 1894, Otto Lubarsch, who supported the theory postulated by Grawitz coined the term hypernephroid tumor, which was amended to hypernephroma by Felix Victor Birch-Hirschfeld to describe these tumours.