Urinary incontinence
[1] Urinary incontinence is common in older women and has been identified as an important issue in geriatric health care.
[4] UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse.
Pelvic surgery, pregnancy, childbirth, attention deficit disorder (ADHD), and menopause are major risk factors.
[11] Treatments that incorporate behavioral therapy are more likely to improve or cure stress, urge, and mixed incontinence, whereas, there is limited evidence to support the benefit of hormones and periurethral bulking agents.
Non-urologic causes may include infection, medication or drugs, psychological factors, polyuria, hydrocephalus,[13] stool impaction, and restricted mobility.
After menopause, estrogen production decreases and, in some women, urethral tissue will demonstrate atrophy, becoming weaker and thinner, possibly playing a role in the development of urinary incontinence.
[16] Stress incontinence is characterized by leaking of small amounts of urine with activities that increase abdominal pressure such as coughing, sneezing, laughing and lifting.
Urge urinary incontinence, is caused by uninhibited contractions of the detrusor muscle, a condition known as overactive bladder syndrome.
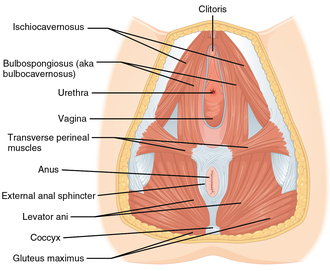
An incompetent urethral sphincter cannot prevent urine from leaking out of the urinary bladder during activities that increase the intraabdominal pressure, such as coughing, sneezing, or laughing.
Continence usually improves within 6 to 12 months after prostate surgery without any specific interventions, and only 5 to 10% of people report persistent symptoms.
The urethral sphincter is the muscular ring that closes the outlet of the urinary bladder preventing urine to pass outside the body.
Any damage to this balance between the detrusor muscle, urethral sphincter, supportive tissue and nerves can lead to some type of incontinence .
Connected to the bottom or next of the bladder, the sphincter is a circular group of muscles that automatically stays contracted to hold the urine in.
[citation needed] Other tests include:[26] People are often asked to keep a diary for a day or more, up to a week, to record the pattern of voiding, noting times and the amounts of urine produced.
The methods include the 1-h pad test, measuring leakage volume; using a voiding diary, counting the number of incontinence episodes (leakage episodes) per day; and assessing of the strength of pelvic floor muscles, measuring the maximum vaginal squeeze pressure.
There are 4 main types of urinary incontinence: Yearly screening is recommended for women by the Women's Preventive Services Initiative (WPSI) and people who test positive in the screening process would need to be referred for further testing to understand how to help treat their condition.
[17] Behavioral therapy involves the use of both suppressive techniques (distraction, relaxation) and learning to avoid foods that may worsen urinary incontinence.
[50][51] They seem to be better than no active treatment in women with stress urinary incontinence, and have similar effects to training of pelvic floor muscles or electrostimulation.
[52] There is some very weak evidence that electrical stimulation that is low in frequency may be helpful in combination with other standard treatments for women with overactive bladder condition,[53] however, the evidence supporting a role for biofeedback combined with pelvic floor muscle training is very weak and likely indicates that biofeedback-assistance is not helpful when included with conservative treatments for overactive bladder.
[52] Preoperative pelvic floor muscle training in men undergoing radical prostatectomy was not effective in reducing urinary incontinence.
[9] Common surgical techniques for stress incontinence include slings, tension-free vaginal tape, bladder suspension, artificial urinary sphincters, among others.
[66] The use of transvaginal mesh implants and bladder slings is controversial due to the risk of debilitating painful side effects such as vaginal erosion.
[68] Urodynamic testing seems to confirm that surgical restoration of vault prolapse can cure motor urge incontinence.
[69] Similarly, there is insufficient long term evidence to be certain about the effectiveness or safety of single-incision sling operations for urinary incontinence in women.
[78] Incontinence is expensive both to individuals in the form of bladder control products and to the health care system and nursing home industry.
[81] Men tend to experience incontinence less often than women, and the structure of the male urinary tract accounts for this difference.
[83] The management of urinary incontinence with pads is mentioned in the earliest medical book known, the Ebers Papyrus (1500 BC).
However, this situation changed some when Kimberly-Clark aggressively marketed adult diapers in the 1980s with actor June Allyson as spokeswoman.
Allyson was initially reticent to participate, but her mother, who had incontinence, convinced her that it was her duty in light of her successful career.
For example, for people who experience urinary incontinence due to stroke, treatment approaches such as physical therapy, cognitive therapy, complementary medicine, and specialized interventions with experienced medical professionals are sometimes suggested, however it is not clear how effective these are at improving incontinence and there is no strong medical evidence to guide clinical practice.