Pulmonary contusion
Children are at especially high risk for the injury because the relative flexibility of their bones prevents the chest wall from absorbing force from an impact, causing it to be transmitted instead to the lung.
[3] Contusion involves hemorrhage in the alveoli (tiny air-filled sacs responsible for absorbing oxygen), but a hematoma is a discrete clot of blood not interspersed with lung tissue.
[14] In general, pulmonary contusion tends to worsen slowly over a few days,[4] but it may also cause rapid deterioration or death if untreated.
[20] Blast lung is severe pulmonary contusion, bleeding, or edema with damage to alveoli and blood vessels, or a combination of these.
[31] Pulmonary contusion results in bleeding and fluid leakage into lung tissue, which can become stiffened and lose its normal elasticity.
The water content of the lung increases over the first 72 hours after injury, potentially leading to frank pulmonary edema in more serious cases.
[20] As a result of these and other pathological processes, pulmonary contusion progresses over time and can cause hypoxia (insufficient oxygen).
[17] Pulmonary contusion is characterized by microhemorrhages (tiny bleeds) that occur when the alveoli are traumatically separated from airway structures and blood vessels.
Fluid accumulation interferes with gas exchange,[34] and can cause the alveoli to fill with proteins and collapse due to edema and bleeding.
Macrophages, neutrophils, and other inflammatory cells and blood components can enter the lung tissue and release factors that lead to inflammation, increasing the likelihood of respiratory failure.
[41] Insufficient inflation of the lungs, which can result from inadequate mechanical ventilation or an associated injury such as flail chest, can also contribute to the ventilation/perfusion mismatch.
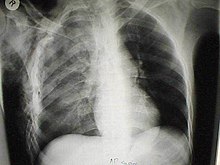
[41] To diagnose pulmonary contusion, health professionals use clues from a physical examination, information about the event that caused the injury, and radiography.
[43] However, in both X-ray and CT a contusion may become more visible over the first 24–48 hours after trauma as bleeding and edema into lung tissues progress.
[39] Monitoring, including keeping track of fluid balance, respiratory function, and oxygen saturation using pulse oximetry is also required as the patient's condition may progressively worsen.
[39] Noninvasive ventilation has advantages over invasive methods because it does not carry the risk of infection that intubation does, and it allows normal coughing, swallowing, and speech.
[15] Pulmonary contusion or its complications such as acute respiratory distress syndrome may cause lungs to lose compliance (stiffen), so higher pressures may be needed to give normal amounts of air[4] and oxygenate the blood adequately.
[15] For people who do require large amounts of intravenous fluid, a catheter may be placed in the pulmonary artery to measure the pressure within it.
[4] Thus, an important part of treatment is pulmonary toilet, the use of suction, deep breathing, coughing, and other methods to remove material such as mucus and blood from the airways.
[61] People with pulmonary contusion, especially those who do not respond well to other treatments, may be positioned with the uninjured lung lower than the injured one to improve oxygenation.
[20] For people who are at especially high risk of developing infections, the sputum can be cultured to test for the presence of infection-causing bacteria; when they are present, antibiotics are used.
[24] Fibrosis of the lungs can occur, resulting in dyspnea (shortness of breath), low blood oxygenation, and reduced functional residual capacity for as long as six years after the injury.
[38] As late as four years post-injury, decreased functional residual capacity has been found in most pulmonary contusion patients studied.
[6] Pulmonary contusion is thought to be the direct cause of death in a quarter to a half of people with multiple injuries (polytrauma) who die.
[73] Children in forceful impacts suffer twice as many pulmonary contusions as adults with similar injury mechanisms, yet have proportionately fewer rib fractures.
[20] Nonetheless, it was the French military surgeon Guillaume Dupuytren who is thought to have coined the term pulmonary contusion in the 19th century.
[70] Pulmonary contusion received further attention during World War II, when the bombings of Britain caused blast injuries and associated respiratory problems in both soldiers and civilians.
[20] Also during this time, studies with animals placed at varying distances from a blast showed that protective gear could prevent lung injuries.
[20] During the Vietnam War, combat again provided the opportunity for study of pulmonary contusion; research during this conflict played an important role in the development of the modern understanding of its treatment.
[20] The condition also began to be more widely recognized in a non-combat context in the 1960s, and symptoms and typical findings with imaging techniques such as X-ray were described.
[15][39] It was first proposed in 1965 that this respiratory insufficiency is most often due to injury of the lung rather than to the chest wall,[20] and a group led by J.K. Trinkle confirmed this hypothesis in 1975.