Blood bank
John Braxton Hicks was the first to experiment with chemical methods to prevent the coagulation of blood at St Mary's Hospital, London, in the late 19th century.
[citation needed] The first non-direct transfusion was performed on March 27, 1914, by the Belgian doctor Albert Hustin, though this was a diluted solution of blood.
The experiments with gelatine, agar, blood serum extracts, starch and beef albumin proved useless.
In June 1915, they made the first important report in the Journal of the American Medical Association that agglutination could be avoided if the blood samples of the donor and recipient were tested before.
[5]Rous was well aware that Austrian physician Karl Landsteiner had discovered blood types a decade earlier, but the practical usage was not yet developed, as he described: "The fate of Landsteiner's effort to call attention to the practical bearing of the group differences in human bloods provides an exquisite instance of knowledge marking time on technique.
[9][10] Canadian Lieutenant Lawrence Bruce Robertson was instrumental in persuading the Royal Army Medical Corps (RAMC) to adopt the use of blood transfusion at the Casualty Clearing Stations for the wounded.
He followed this up with four subsequent transfusions in the following months, and his success was reported to Sir Walter Morley Fletcher, director of the Medical Research Committee.
Robertson went on to establish the first blood transfusion apparatus at a Casualty Clearing Station on the Western Front in the spring of 1917.
[11] Oswald Hope Robertson, a medical researcher and U.S. Army officer, worked with Rous at the Rockefeller between 1915 and 1917, and learned the blood matching and preservation methods.
[12] He was attached to the RAMC in 1917, where he was instrumental in establishing the first blood banks, with soldiers as donors, in preparation for the anticipated Third Battle of Ypres.
[13] He used sodium citrate as the anticoagulant, and the blood was extracted from punctures in the vein, and was stored in bottles at British and American Casualty Clearing Stations along the Front.
[11] Geoffrey Keynes, a British surgeon, developed a portable machine that could store blood to enable transfusions to be carried out more easily.
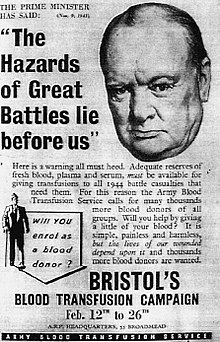
The world's first blood donor service was established in 1921 by the secretary of the British Red Cross, Percy Lane Oliver.
Similar systems were established in other cities including Sheffield, Manchester and Norwich, and the service's work began to attract international attention.
[15] Vladimir Shamov and Sergei Yudin in the Soviet Union pioneered the transfusion of cadaveric blood from recently deceased donors.
With support from the Department of Health of the Spanish Republican Army, Duran established a blood bank for the use of wounded soldiers and civilians.
[18] Frederic Durán-Jordà fled to Britain in 1938, and worked with Janet Vaughan at the Royal Postgraduate Medical School at Hammersmith Hospital to create a system of national blood banks in London.
[22] Charles R. Drew was appointed medical supervisor, and he was able to transform the test tube methods into the first successful mass production technique.
Stetson discovered the Rh blood group system, which was found to be the cause of the majority of transfusion reactions up to that time.
Units of WB and RBC are both kept refrigerated at 33.8 to 42.8 °F (1.0 to 6.0 °C), with maximum permitted storage periods (shelf lives) of 35 and 42 days respectively.
The layer between the red cells and the plasma is referred to as the buffy coat and is sometimes removed to make platelets for transfusion.
Notably, U.S. hospitals spend more on dealing with the consequences of transfusion-related complications than on the combined costs of buying, testing/treating, and transfusing their blood.
[38] In general, there are not yet any in vitro tests to assess quality deterioration or preservation for specific units of RBC blood product prior to their transfusion, though there is exploration of potentially relevant tests based on RBC membrane properties such as erythrocyte deformability[39] and erythrocyte fragility (mechanical).
[43] Although as noted the primary inventory-management approach is first in, first out (FIFO) to minimize product expiration, there are some deviations from this policy—both in current practice as well as under research.
For example, exchange transfusion of RBC in neonates calls for use of blood product that is five days old or less, to "ensure" optimal cell function.
[44] Also, some hospital blood banks will attempt to accommodate physicians' requests to provide low-aged RBC product for certain kinds of patients (e.g. cardiac surgery).