Traumatic brain injury
TBI can result in physical, cognitive, social, emotional and behavioral symptoms, and outcomes can range from complete recovery to permanent disability or death.
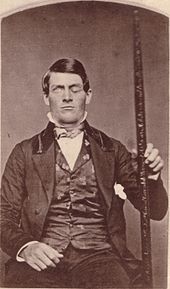
[15] A penetrating, or open, head injury occurs when an object pierces the skull and breaches the dura mater, the outermost membrane surrounding the brain.
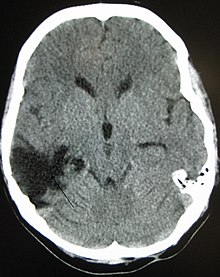
[24] Damage from TBI can be focal or diffuse, confined to specific areas or distributed in a more general manner, respectively;[25] however, it is common for both types of injury to exist in a given case.
[41] Other symptoms of mild TBI include headache, vomiting, nausea, lack of motor coordination, dizziness, difficulty balancing,[42] lightheadedness, blurred vision or tired eyes, ringing in the ears, bad taste in the mouth, fatigue or lethargy, and changes in sleep patterns.
[51] Signs of increased ICP include decreasing level of consciousness, paralysis or weakness on one side of the body, and a blown pupil, one that fails to constrict in response to light or is slow to do so.
[51] Cushing's triad, a slow heart rate with high blood pressure and respiratory depression is a classic manifestation of significantly raised ICP.
[70] A large percentage of the people killed by brain trauma do not die right away but rather days to weeks after the event;[71] rather than improving after being hospitalized, some 40% of TBI patients deteriorate.
[73] These secondary processes can dramatically worsen the damage caused by primary injury[63] and account for the greatest number of TBI deaths occurring in hospitals.
[51] Diagnosis is suspected based on lesion circumstances and clinical evidence, most prominently a neurological examination, for example checking whether the pupils constrict normally in response to light and assigning a Glasgow Coma Score.
[10] Functional imaging can measure cerebral blood flow or metabolism, inferring neuronal activity in specific regions and potentially helping to predict outcome.
[63] Due to the possibility that repeatedly "heading" a ball practicing soccer could cause cumulative brain injury, the idea of introducing protective headgear for players has been proposed.
[96] Further research is required to determine the effectiveness and clinical importance of positioning the head at different angles (degrees of head-of-bed elevation) while the person is being treated in intensive care.
[98] A more accurate way to measure ICP is to place a catheter into a ventricle of the brain,[39] which has the added benefit of allowing cerebrospinal fluid to drain, releasing pressure in the skull.
[99] Hypertonic saline can improve ICP by reducing the amount of cerebral water (swelling), though it is used with caution to avoid electrolyte imbalances or heart failure.
[106] Diuretics, drugs that increase urine output to reduce excessive fluid in the system, may be used to treat high intracranial pressures, but may cause hypovolemia (insufficient blood volume).
[109][110] There is no strong evidence that the following pharmaceutical interventions should be recommended to routinely treat TBI: magnesium, monoaminergic and dopamine agonists, progesterone, aminosteroids, excitatory amino acid reuptake inhibitors, beta-2 antagonists (bronchodilators), haemostatic and antifibrinolytic drugs.
[23] Blood pressure may be kept at an artificially high level under controlled conditions by infusion of norepinephrine or similar drugs; this helps maintain cerebral perfusion.
[120] DC performed hours or days after TBI in order to control persistently high intracranial pressures (secondary DC), although can reduce intracranial pressure and length of stay in ICU, but have worse Glasgow Coma Scale (GCS) scores, and high chances of death, vegetative state, or severe disability when compared to those receiving standard medical therapies.
[124] Treatment of neuropsychiatric symptoms such as emotional distress and clinical depression may involve mental health professionals such as therapists, psychologists, and psychiatrists, while neuropsychologists can help to evaluate and manage cognitive deficits.
In addition, the orthosis must be designed by the orthotist in such a way that it achieves the effectiveness of the necessary levers, matching the gait pattern, in order to support the proprioceptive approaches of physiotherapy.
[76] Other influences that may affect recovery include pre-injury intellectual ability, coping strategies, personality traits, family environment, social support systems and financial circumstances.
The results of traumatic brain injury vary widely in type and duration; they include physical, cognitive, emotional, and behavioral complications.
[92] Post-concussion syndrome, a set of lasting symptoms experienced after mild TBI, can include physical, cognitive, emotional and behavioral problems such as headaches, dizziness, difficulty concentrating, and depression.
[157][158][159][160] These may include emotional instability, depression, anxiety, hypomania, mania, apathy, irritability, problems with social judgment, and impaired conversational skills.
[63] Deaths have declined due to improved treatments and systems for managing trauma in societies wealthy enough to provide modern emergency and neurosurgical services.
[181] Ancient Greek physicians including Hippocrates understood the brain to be the center of thought, probably due to their experience observing the effects of head trauma.
[178] Explosives used in World War I caused many blast injuries; the large number of TBIs that resulted allowed researchers to learn about localization of brain functions.
[197] Although neuroprotection methods to decrease secondary injury have been the subject of interest follows TBI, trials to test agents that could halt these cellular mechanisms have met largely with failure as of 2008.
Microdialysis allows ongoing sampling of extracellular fluid for analysis of metabolites that might indicate ischemia or brain metabolism, such as glucose, glycerol, and glutamate.
The findings of a 2012 Cochrane systematic review does not justify the routine use of hyperbaric oxygen therapy to treat people recovering from a traumatic brain injury.