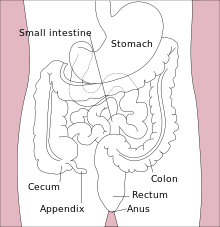
Appendicitis
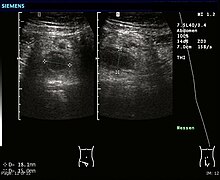
[4] Although ultrasound may aid in diagnosis, its main role is in identifying important differentials, such as ovarian pathology in females or mesenteric adenitis in children.
[13] The causative agents include bezoars, foreign bodies, trauma,[21][22] lymphadenitis and, most commonly, calcified fecal deposits that are known as appendicoliths or fecaliths.
[26] Fecal stasis and arrest may play a role, as demonstrated by people with acute appendicitis having fewer bowel movements per week compared with healthy controls.
[24][27] The occurrence of a fecalith in the appendix was thought to be attributed to a right-sided fecal retention reservoir in the colon and a prolonged transit time.
Studies have implicated a transition to a Western diet lower in fiber in rising frequencies of appendicitis as well as the other aforementioned colonic diseases in these communities.
[35] The physician will ask questions to get the health history, assess the patient's symptoms, do a complete physical exam, and order both laboratory and imaging tests.
[37] Typical appendicitis is characterized by a migratory right iliac fossa pain associated with nausea, and anorexia, which can occur with or without vomiting and localized muscle stiffness/ generalized guarding.
[38] The combination of migrated umbilical pain to the right lower quadrant, loss of appetite for food, nausea, unsustained vomiting, and mild fever is classic.
Irritation of the peritoneum (inside lining of the abdominal wall) can lead to increased pain on movement, or jolting, for example going over speed bumps.
[49] Several routine and non-routine laboratory tests have been investigated for discriminating simple and complicated appendicitis, but their diagnostic accuracy is uncertain.
Other secondary sonographic signs of acute appendicitis include the presence of echogenic mesenteric fat surrounding the appendix and the acoustic shadowing of an appendicolith.
Also, false-negative findings are more common in adults where larger amounts of fat and bowel gas make visualizing the appendix technically difficult.
Some of these conditions include inflammation of lymph nodes near the appendix or pain originating from other pelvic organs such as the ovaries or Fallopian tubes.
Although some concerns about interpretation are identified, a 2019 Cochrane review found that the sensitivity and specificity of CT for the diagnosis of acute appendicitis in adults was high.
[64][65] The accurate diagnosis of appendicitis is multi-tiered, with the size of the appendix having the strongest positive predictive value, while indirect features can either increase or decrease sensitivity and specificity.
[66] However, because the appendix can be filled with fecal material, causing intraluminal distention, this criterion has shown limited utility in more recent meta-analyses.
First-trimester pregnancies are usually not candidates for MRI, as the fetus is still undergoing organogenesis, and there are no long-term studies to date regarding its potential risks or side effects.
[70][71] Plain abdominal films may be useful for the detection of ureteral calculi, small bowel obstruction, or perforated ulcer, but these conditions are rarely confused with appendicitis.
Even for clinically certain appendicitis, routine histopathology examination of appendectomy specimens is of value for identifying unsuspected pathologies requiring further postoperative management.
Other obstetrical/ gynecological causes of similar abdominal pain in women include pelvic inflammatory disease, ovarian torsion, menarche, dysmenorrhea, endometriosis, and Mittelschmerz (the passing of an egg in the ovaries approximately two weeks before menstruation).
While antibiotics are safe and effective for treating uncomplicated appendicitis,[16][7][85] 31% of people had a recurrence within a year and required an eventual appendectomy.
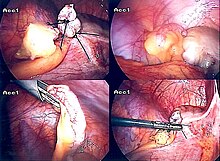
In case of complicated appendicitis managed by an emergency open appendectomy, abdominal drainage (a temporary tube from the abdomen to the outside to avoid abscess formation) may be inserted, but this may increase the hospital stay.
[97] In pediatric patients, the high mobility of the cecum allows externalization of the appendix through the umbilicus, and the entire procedure can be performed with a single incision.
Laparoscopic-assisted transumbilical appendectomy is a relatively recent technique but with a long published series and very good surgical and aesthetic results.
[14] After surgery, the patient will be transferred to a postanesthesia care unit, so their vital signs can be closely monitored to detect anesthesia- or surgery-related complications.
Most individuals will be offered clear liquids the day after the surgery, then progress to a regular diet when the intestines start to function correctly.
Recovery time depends on age, condition, complications, and other circumstances, including the amount of alcohol consumption, but usually is between 10 and 28 days.
Clinical understanding progressed in the 18th and 19th centuries, marked by Lorenz Heister's autopsy findings, Claudius Aymand's surgical intervention, and J. Mestivier's operation for appendicitis.
Modern appendectomy techniques evolved in the early 20th century, coinciding with advancements in pathology, notably demonstrated by Ludwig Aschoff in 1908.
[14] Appendicitis is one of the most frequent diagnoses for emergency department visits resulting in hospitalization among children ages 5–17 years in the United States.