Calcium metabolism
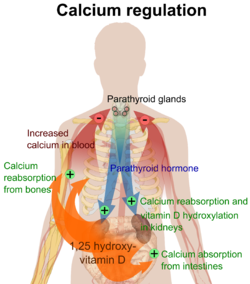
PTH is released by the chief cells of the parathyroid glands when the plasma calcium level falls below the normal range in order to raise it; calcitonin is released by the parafollicular cells of the thyroid gland when the plasma level of calcium is above the normal range in order to lower it.
[3] The average adult body contains in total approximately 1 kg, 99% in the skeleton in the form of calcium phosphate salts.
It is therefore the plasma ionized calcium level which is tightly regulated to remain within very narrow limits by homeostatic negative feedback systems.
The ionized calcium can be determined directly by colorimetry, or it can be read off from nomograms, though the usefulness of the latter is limited when the pH and protein content of the plasma deviate widely from the normal.
It readily binds to proteins, particularly those with amino acids whose side chains terminate in carboxyl (-COOH) groups (e.g. glutamate residues).
[6] Relatively small decreases in the plasma ionized calcium levels (hypocalcemia) cause these channels to leak sodium into the nerve cells or axons, making them hyper-excitable (positive bathmotropic effect), thus causing spontaneous muscle spasms (tetany) and paraesthesia (the sensation of "pins and needles") of the extremities and round the mouth.
This can therefore serve as a very effective intracellular signal (or "second messenger") in a variety of circumstances, including muscle contraction, the release of hormones (e.g. insulin from the beta cells in the pancreatic islets) or neurotransmitters (e.g. acetylcholine from pre-synaptic terminals of nerves) and other functions.
The troponin's 3D structure changes as a result, causing the tropomyosin to which it is attached to be rolled away from the myosin-binding sites on the actin molecules that form the back-bone of the thin filaments.
Myosin can then bind to the exposed myosin-binding sites on the thin filament, to undergo a repeating series of conformational changes called the cross-bridge cycle, for which ATP provides the energy.
The calcium that is most readily absorbed is found in dairy products (72%), vegetables (7%), grains (5%), legumes (4%), fruit (3%), protein (3%).
Calcium release from bone is regulated by parathyroid hormone in conjunction with calcitriol manufactured in the kidney under the influence of PTH.
[22] The active absorption of calcium from the gut is regulated by the calcitriol (or 1,25 dihydroxycholecalciferol, or 1,25 dihydroxyvitamin D3) concentration in the blood.
Under the influence of ultraviolet light on the skin, cholesterol is converted to previtamin D3 which spontaneously isomerizes to vitamin D3 (or cholecalciferol).
[note 1] However, parathyroid hormone has a greater effect on the quantity of phosphate ions (HPO42−) excreted in the urine.
It processes vitamin D3 into calcitriol, the active form that is most effective in promoting the intestinal absorption of calcium.
When the concentration of calcium rises, the parafollicular cells of the thyroid gland increase their secretion of calcitonin, a polypeptide hormone, into the blood.
The low levels of PTH also inhibit the formation of calcitriol (not to be confused with calcitonin) from cholecalciferol (vitamin D3) by the kidneys.
The reduction in the blood calcitriol concentration acts (comparatively slowly) on the epithelial cells (enterocytes) of the duodenum, inhibiting their ability to absorb calcium from the intestinal contents.
[2][5][28][29] The low calcitriol levels also act on bone causing the osteoclasts to release fewer calcium ions into the blood plasma.
The high plasma PTH levels inhibit calcium loss via the urine while stimulating the excretion of phosphate ions via that route.