Hereditary cancer syndrome
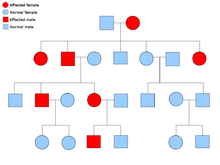
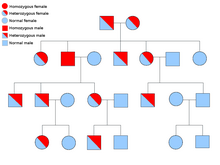
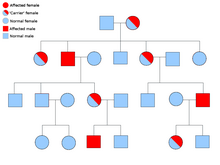
A heterozygous individual and a person with two normal alleles (homozygous) will have a 50% chance of producing an affected child.
[citation needed] Fanconi anemia is a disorder with a wide clinical spectrum, including: early onset and increased risk of cancer; bone marrow failure; and congenital abnormalities.
The most prominent manifestations of this disorder are those related to hematopoeisis (production of blood by the bone marrow); these include aplastic anemia, myelodysplastic syndrome and acute myeloid leukemia.
Congenital abnormalities include: skeletal anomalies (especially those affecting the hands), cafe au lait spots and hypopigmentation.
To date, the genes known to cause FA are: FANCA, FANCB, FANCC, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCJ, FANCL, FANCM, FANCN, FANCO, FANCP and BRCA2 (previously known as FANCD1).
[12][13][14][15][16] Familial adenomatous polyposis (FAP) is an autosomal dominant syndrome that greatly increases the risk of colorectal cancer.
An individual with this disease will have hundreds to thousands of benign adenomas throughout their colon, which will in most cases progress to cancer.
BRCA1 and BRCA2 are both tumor suppressor genes implicated in maintaining and repairing DNA, which in turn leads to genome instability.
These short repetitive sequences of DNA become unstable, leading to a state of microsatellite instability (MSI).
Mutated microsatellites are often found in genes involved in tumor initiation and progression, and MSI can enhance the survival of cells, leading to cancer.
The reason for the large clinical spectrum of this disorder may be due to other gene mutations that modify the disease.
MUTYH-associated polyposis shares most of its clinical features with FAP; the difference is that it is an autosomal recessive disorder caused by mutations in the MUTYH DNA repair gene.
The most common skeletal abnormalities occur in the head and face, but other areas are often affected such as the rib cage.
[32][33] Von Hippel–Lindau disease is a rare, autosomal dominant genetic condition that predisposes individuals to benign and malignant tumors.
The most common tumors in Von Hippel–Lindau disease are central nervous system and retinal hemangioblastomas, clear cell renal carcinomas, pheochromocytomas, pancreatic neuroendocrine tumours, pancreatic cysts, endolymphatic sac tumors and epididymal papillary cystadenomas.
[citation needed] In addition to cancer, some genetic mutations that cause xeroderma pigmentosum are associated with neurodegeneration.
Xeroderma pigmentosum may be caused by genetic mutations in 8 genes, which produce the following enzymes: XPA, XPB, XPC, XPD, XPE, XPF, XPG and Pol η. XPA-XPF are nucleotide excision repair enzymes that repair UV light-damaged DNA and faulty proteins will allow the buildup of mutations caused by UV light.
Mutations in this gene will produce a faulty pol η enzyme that cannot replicate DNA with UV light damage.
sebaceous adenomas) [48] Genetic testing can be used to identify mutated genes or chromosomes that are passed through generations.
However, before genes are tested for mutations the patient usually must go to a health care provider and go through a one-on-one consultation, where they discuss both the personal and family history of cancer.
The medical professional can then assess the likelihood of the patient having the mutation and can guide them through the process that is genetic screening.
[73] Regular breast screening is also recommended for women diagnosed with BRCA mutations, as well as that, recent studies show that men with increased risks of developing prostate cancer due to BRCA mutations can decrease their risk by taking aspirin.
[74] Aspirin is hugely beneficial in lowering cancer prevalence; however, it must be taken regularly over at least a five-year period to have any effect.
[76] 1 in 40 Ashkenazi Jews have a BRCA mutation, this is a huge contrast from the general population in the United States where 1 in 400 people are affected.