Prostate cancer
This most-advanced stage of the disease, called castration-resistant prostate cancer, is treated with continued hormone therapy alongside the chemotherapy drug docetaxel.
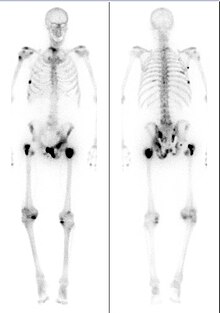
[4] Advanced prostate tumors can metastasize to nearby lymph nodes and bones, particularly in the pelvis, hips, spine, ribs, head, and neck.
[12] Medical guidelines generally recommend against screening for men over age 70, or with a life expectancy of less than 10 years, as a newly diagnosed prostate cancer is unlikely to impact their natural lifespan.
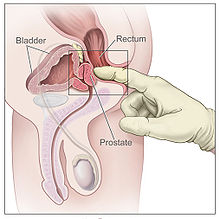
One common procedure is the digital rectal examination, in which a doctor inserts a lubricated finger into the rectum to feel the nearby prostate.
[25] Several urological societies' guidelines recommend magnetic resonance imaging (MRI) to evaluate the prostate for potential tumors in men with high PSA levels.
[32] The AJCC then combines the TNM scores, Gleason grade group, and results of the PSA blood test to categorize cancer cases into one of four stages, and their subdivisions.
Stage III is the designation for any of three higher risk factors: IIIA is for a PSA level about 20 ng/mL; IIIB is for T3 or T4 tumors; IIIC is for a Gleason grade group of 5.
[39] Men diagnosed with low-risk cases of prostate cancer often defer treatment and are monitored regularly for cancer progression by active surveillance, which involves testing for tumor growth at fixed intervals by PSA tests (around every six months), digital rectal exam (annually), and MRI or repeat biopsies (every one to three years).
[49] Radical prostatectomy aims to surgically remove the cancerous part of the prostate, along with the seminal vesicles, and the end of the vas deferens (the duct that delivers sperm from the testes).
[52] Both for cancer progression outcomes and surgical side effects, the skill and experience of the individual surgeon doing the procedure are among the greatest determinants of success.
The first line of treatment typically involves GnRH agonists like leuprolide, goserelin, or triptorelin by injection monthly or less frequently as needed.
[58][57] GnRH agonists cause a brief rise in testosterone levels at treatment initiation, which can worsen disease in people with significant symptoms of metastases.
CRPC tumors continuously evolve resistance to treatments, necessitating several lines of therapy, each used in sequence to extend survival.
The standard of care is the chemotherapy docetaxel along with antiandrogen drugs, namely the androgen receptor antagonists enzalutamide, apalutamide, and darolutamide, as well as the testosterone production inhibitor abiraterone acetate.
These are typically treated with appetite-increasing drugs – megestrol acetate or corticosteroids – antiemetics, or treatments that focus on underlying gastrointestinal issues.
[73] Organ damage and metastases in the lymph nodes can lead to uncomfortable accumulation of fluid (called lymphedema) in the genitals or lower limbs.
[75] When added to normal prostate cancer treatments, psychological interventions such as psychoeducation and cognitive behavioral therapy can help reduce anxiety, depression, and general distress.
[76] As those severely ill with metastatic prostate cancer approach the end of their lives, most experience confusion and may hallucinate or have trouble recognizing loved ones.
[85] These cells can spread through the lymphatic system to nearby lymph nodes, or through the bloodstream to the bone marrow and (more rarely) other body sites.
[100] Regular vigorous exercise may reduce one's chance of developing advanced prostate cancer, as can several dietary interventions.
[96][102] Conversely, those who consume high levels of dietary fats, polycyclic aromatic hydrocarbons (from cooking red meats), or calcium may be at an increased risk of developing advanced prostate cancer.
[106] A prostate mass was first described in 1817 by the English surgeon George Langstaff, following the autopsy of a man who had died at age 68 with lower-body pain and urinary issues.
[111] This was improved upon by Patrick C. Walsh's 1983 description of a retropubic prostatectomy approach that avoided damage to the nerves near the prostate, preserving erectile function.
[111][113] Radiation therapy for prostate cancer was used occasionally in the early 20th century, with radium implanted into the urethra or rectum to reduce the tumor size and associated symptoms.
[114] The observation that the testicles (and the hormones they secrete) influence prostate size was made as early as the late 18th century via castration experiments in animals.
In 1941, Charles B. Huggins and Clarence V. Hodges published two studies using surgical castration or oral estrogen to reduce androgen levels and improve prostate cancer symptoms.
[115] Systemic chemotherapy for prostate cancer has been studied since the 1950s but clinical trials failed to show benefits in most people who receive the drugs.
[118] In 1996, the US Food and Drug Administration approved the systemic chemotherapy mitoxantrone for those with castration-resistant prostate cancer based on trials showing that it improved symptoms even though it failed to enhance survival.
[127] These genetically engineered mouse models typically use a Cre recombinase system to disrupt tumor suppressors or activate oncogenes specifically in prostate cells.
[128] As of 2024[update] studies exploring the relationship between ejaculation frequency and prostate cancer risk are inconclusive and age, urinary health, and lifestyle are important factors to consider.