Chylomicron retention disease
[3] Physical symptoms of CMRD involving the development and function of the gastrointestinal tract and nervous system typically manifest between infancy and adolescence.
[5] Chylomicron retention disease is an autosomal homozygous recessive disorder arising from mutations in the gene encoding the Sar1B GTPase.
In CMRD, a mutation of this genomic sequence affects the Sar1B enzyme's ability to interact with Guanine Exchange Factors (GEFs) and GTP-Activating Proteins (GAPs).
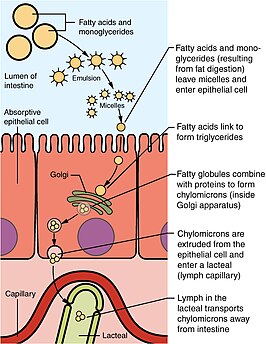
[citation needed] During digestion, fats, or triglycerides(TGs), are enzymatically catabolized by lipases into two fatty acids and a monoglyceride molecule.
The pre-chylomicrons are then packaged into PCTV to be transported to the Golgi apparatus for additional maturation prior to exocytosis into the lymphatic system.
[8] In chylomicron retention disease, the PCTV vesicles are competent for budding from the ER membrane but are defective for fusion with the cis-golgi body.
Assessment of hypobetalipoproteinemia relies chiefly on blood lipid analysis following a 12-hr fasting period.
[5] Because patient outcomes rely on early diagnosis, it is recommended that candidates for the disorder should receive lipid panel testing prior to 6 months of age.
[10] It is recommended that patients with CMRD follow a strict low-fat diet in addition to fat-soluble vitamin supplementation.
Long-term treatment plans center around dietary management, but because long term results have not been documented due to a lack of thorough research, careful monitoring of the disease is required.
In adulthood, past eighteen years of age, echocardiograms are recommended to track heart activity.
Careful regulation of diet and nutrition are required for management of CMRD since the disease results from the poor absorption of nutrients from food.
[citation needed] Charlotte Anderson first published a description of the disorder in 1961, where she observed a seven month old girl who developed intestinal mucosa filled with fat droplets.
In 2003, Jones and colleagues identified mutations in the SAR1B gene, which transcripts the SAR1B protein involved in COPII transport and proposed this was the molecular defect of the disorder.