Cortisol
[2] By a diurnal cycle, cortisol is released and increases in response to stress and a low blood-glucose concentration.
[1] It functions to increase blood sugar through gluconeogenesis, suppress the immune system, and aid in the metabolism of calories.
All of these metabolic steps have the net effect of increasing blood glucose levels, which fuel the brain and other tissues during the fight-or-flight response.
[6] In general, cortisol stimulates gluconeogenesis (the synthesis of 'new' glucose from non-carbohydrate sources, which occurs mainly in the liver, but also in the kidneys and small intestine under certain circumstances).
[7] Cortisol also plays an important, but indirect, role in liver and muscle glycogenolysis (the breaking down of glycogen to glucose-1-phosphate and glucose) which occurs as a result of the action of glucagon and adrenaline.
[10] This is in contrast to cortisol's effect in the skeletal muscle where glycogenolysis (breakdown of glycogen into glucose molecules) is promoted indirectly through catecholamines.
[14] The usual explanation to account for this apparent discrepancy is that the raised blood glucose concentration (through the action of cortisol) will stimulate insulin release.
Insulin stimulates lipogenesis, so this is an indirect consequence of the raised cortisol concentration in the blood but it will only occur over a longer time scale.
Low-dose topical hydrocortisone, available as a nonprescription medicine in some countries, is used to treat skin problems such as rashes and eczema.
The activation of the stress system (and resulting increase in cortisol and Th2 shift) seen during an infection is believed to be a protective mechanism which prevents an over-activation of the inflammatory response.
Cortisol downregulates the expression of the IL2 receptor IL-2R on the surface of the helper T-cell which is necessary to induce a Th1 'cellular' immune response, thus favoring a shift towards Th2 dominance and the release of the cytokines listed above which results in Th2 dominance and favors the 'humoral' B-cell mediated antibody immune response.
A larger number of lymphocytes in the lymph nodes, bone marrow, and skin means the body is increasing its humoral immune response.
Finally antibodies can also activate complement molecules which can combine in various ways to promote opsonization or even act directly to lyse a bacteria.
[22][23][24] This viral strategy can have severe consequences for the host (human that is infected by the virus), as cortisol is essential for regulating various physiological processes, such as metabolism, blood pressure, inflammation, and immune response.
A lack of cortisol can result in a condition called adrenal insufficiency, which can cause symptoms such as fatigue, weight loss, low blood pressure, nausea, vomiting, and abdominal pain.
Therefore, by suppressing cortisol production, some viruses can escape the immune system and weaken the host's overall health and resilience.
[1][27] Cortisol also increases glycogen synthesis (glycogenesis) in the liver, storing glucose in easily accessible form.
The mechanism behind this is two-fold: cortisol stimulates the production of RANKL by osteoblasts which stimulates, through binding to RANK receptors, the activity of osteoclasts – cells responsible for calcium resorption from bone – and also inhibits the production of osteoprotegerin (OPG) which acts as a decoy receptor and captures some RANKL before it can activate the osteoclasts through RANK.
[49] Although the timing of fetal cortisol concentration elevation in sheep may vary somewhat, it averages about 11.8 days before the onset of labor.
[50] In several livestock species (e.g. cattle, sheep, goats, and pigs), the surge of fetal cortisol late in gestation triggers the onset of parturition by removing the progesterone block of cervical dilation and myometrial contraction.
Exposure of fetuses to cortisol during gestation can have a variety of developmental outcomes, including alterations in prenatal and postnatal growth patterns.
These results suggest that gestational exposure to cortisol in fetuses has important potential fetal programming effects on both pre and postnatal growth in primates.
Measured cortisol levels, and therefore reference ranges, depend on the sample type, analytical method used, and factors such as age and sex.
[76][77][78][79] Transcortin particles are too large to pass through this barrier,[80] that consists of epithelial cell layers of the oral mucosa and salivary glands.
Cortisol even has a negative feedback effect on interleukin-1[17]—especially useful to treat diseases that force the hypothalamus to secrete too much CRH, such as those caused by endotoxic bacteria.
[98] Ascorbic acid presence, particularly in high doses has also been shown to mediate response to psychological stress and speed the decrease of the levels of circulating cortisol in the body post-stress.
[112][113] In humans, the medulla of the adrenal gland lies under its cortex, mainly secreting the catecholamines adrenaline (epinephrine) and noradrenaline (norepinephrine) under sympathetic stimulation.
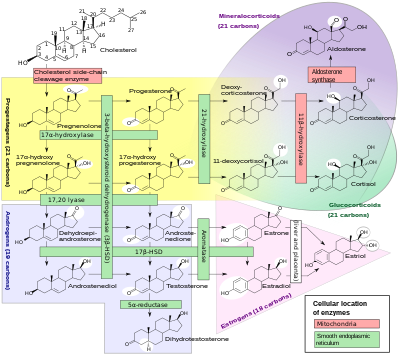
ACTH increases the concentration of cholesterol in the inner mitochondrial membrane, via regulation of the steroidogenic acute regulatory protein.
It also stimulates the main rate-limiting step in cortisol synthesis, in which cholesterol is converted to pregnenolone and catalyzed by Cytochrome P450SCC (side-chain cleavage enzyme).
[118] An alteration in 11-beta HSD1 has been suggested to play a role in the pathogenesis of obesity, hypertension, and insulin resistance known as metabolic syndrome.