Urinary tract infection
[2] Risk factors include female anatomy, sexual intercourse, diabetes, obesity, catheterisation, and family history.
[7] Urinary tract infections have been described since ancient times with the first documented description in the Ebers Papyrus dated to c. 1550 BC.
[28] Because of the lack of more obvious symptoms, when females under the age of two or uncircumcised males less than a year exhibit a fever, a culture of the urine is recommended by many medical associations.
[11] It is reasonable to obtain a urine culture in those with signs of systemic infection that may be unable to report urinary symptoms, such as when advanced dementia is present.
have several times been found as the primary cause of urinary tract infection, suggested related to broad treatment with cephalosporin antibiotics against which they are tolerant.
[40] Condom use without spermicide or use of birth control pills does not increase the risk of uncomplicated urinary tract infection.
[42] As a woman's estrogen levels decrease with menopause, her risk of urinary tract infections increases due to the loss of protective vaginal flora.
[42] Additionally, vaginal atrophy that can sometimes occur after menopause is associated with recurrent urinary tract infections.
While bacteria is commonly present in the urine of older males this does not appear to affect the risk of urinary tract infections.
The risk of bacteriuria (bacteria in the urine) is between three and six percent per day and prophylactic antibiotics are not effective in decreasing symptomatic infections.
[42] The risk of an associated infection occurs liniearly for enteric bacteria,[45][35] and can be decreased by catheterizing only when necessary, using aseptic technique for insertion, and maintaining unobstructed closed drainage of the catheter.
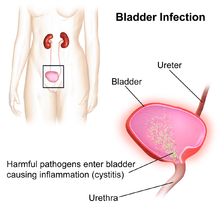
[10] In children UTIs are associated with vesicoureteral reflux (an abnormal movement of urine from the bladder into ureters or kidneys) and constipation.
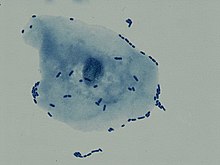
[7] It is believed that the bacteria are usually transmitted to the urethra from the bowel, with females at greater risk due to their anatomy.
[7] Escherichia coli is the single most common microorganism, followed by Klebsiella and Proteus spp., to cause urinary tract infection.
Urine culture is deemed positive if it shows a bacterial colony count of greater than or equal to 103 colony-forming units per mL of a typical urinary tract organism.
[4] As symptoms can be vague and without reliable tests for urinary tract infections, diagnosis can be difficult in the elderly.
The use of "urine bags" to collect samples is discouraged by the World Health Organization due to the high rate of contamination when cultured, and catheterization is preferred in those not toilet trained.
However, because there is a lack of effective treatment if problems are found, others such as the National Institute for Health and Care Excellence only recommends routine imaging in those less than six months old or who have unusual findings.
[56] Interstitial cystitis (chronic pain in the bladder) may be considered for people who experience multiple episodes of UTI symptoms but urine cultures remain negative and not improved with antibiotics.
[58] Hemorrhagic cystitis, characterized by blood in the urine, can occur secondary to a number of causes including: infections, radiation therapy, underlying cancer, medications and toxins.
[7] In those with benign prostatic hyperplasia urinating in a sitting position appears to improve bladder emptying[62] which might decrease urinary tract infections in this group.
[75] When used as an adjuvant to antibiotics and other standard treatments, cranberry supplements decrease the number of UTIs in people who get them frequently.
[79] Cranberry supplements are also high in sugar content, which may worsen the risks associated with UTIs in patients with diabetes mellitus.
Phenazopyridine is occasionally prescribed during the first few days in addition to antibiotics to help with the burning and urgency sometimes felt during a bladder infection.
[82] However, it is not routinely recommended due to safety concerns with its use, specifically an elevated risk of methemoglobinemia (higher than normal level of methemoglobin in the blood).
[54] The Food and Drug Administration (FDA) recommends against the use of fluoroquinolones, including a Boxed Warning, when other options are available due to higher risks of serious side effects, such as tendinitis, tendon rupture and worsening of myasthenia gravis.
[54][93] The Infectious Diseases Society of America states this due to the concern of generating resistance to this class of medication.
[7] Among children, urinary tract infections are most common in uncircumcised males less than three months of age, followed by females less than one year.
[28] Urinary tract infections have been described since ancient times with the first documented description in the Ebers Papyrus dated to c. 1550 BC.
[116] Effective treatment did not occur until the development and availability of antibiotics in the 1930s, before which time herbs, bloodletting and rest were recommended.