Deep brain stimulation
[1] As a first approximation, DBS is thought to mimic the clinical effects of lesioning,[8] likely by attenuating (pathologically elevated) information flow through affected brain networks.
The IPG is a battery-powered neurostimulator encased in a titanium housing, which sends electrical pulses to the brain that interfere with neural activity at the target site.
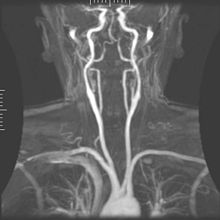
The leads are two coiled wires insulated in polyurethane with four platinum-iridium electrodes that allow delivery of electric charge from the battery back implanted in the chest wall.
The leads, in turn, are connected to the battery by an insulated extension wire which travels from the chest wall superiorly along the back of the neck below the skin, behind the ear, and finally enters the skull through a surgically made burr hole to terminate in the deep nuclei of the brain.
[11] After surgery, battery dosage is titrated to individual symptoms, a process which requires repeat visits to a clinician for readjustment.
A hole about 14 mm in diameter is drilled in the skull and the probe electrode is inserted stereotactically, using either frame-based or frameless stereotaxis.
[citation needed] Though not common, placement can be accompanied by intracranial hemorrhage, infection or obstructive hydrocephalus, which may require repositioning or a stay in the neurological intensive care unit.
Long term negative effects of the device include an increased risk of decreased mental function and dementia beyond that typically seen with neurodegenerative disorders.
A 2024 Danish meta-analysis found improvements, primarily in motor function, with deep brain stimulation with antiparkinsonian drugs against a variety of controls.
Serious adverse events relating to hardware and perioperative complications were increased, but data were insufficient to assess the important outcome of all-cause mortality.
Recent metaanalytical evidence suggests that multiple targets along the circuitry of the cerebellothalamic pathway (also referred to as the dentatorubrothalamic or dentatothalamic tract) are similarly effective, i.e. modulating the cerebellar inflows into the thalamus may be key for therapeutic efficacy,[24][25] for a review see.
This delayed response is thought to reflect the complexity of motor circuits involved in dystonia and the long-term plastic changes required for symptom relief.
DBS for dystonia is generally considered safe, but like all neuromodulation therapies, it comes with potential risks, including infection, hardware complications, or stimulation-related side effects such as speech difficulties.
Ongoing research aims to optimize DBS targeting and stimulation settings to enhance outcomes for individuals with different types of dystonia.
[36] In Europe, the CE Mark for DBS for OCD was active from 2009 to 2022 but not renewed thereafter due to a lack of coverage by government health agencies.
[34] Building upon the ablative lesion cases carried out by Rolf Hassler and colleagues,[44] Visser-Vandewalle chose the intersection between the centromedian, parafascicular and ventrooralis internus nuclei of the thalamus as her DBS target.
Despite widely publicized early successes, DBS remains a highly experimental procedure for treating Tourette's, and more study is needed to determine whether long-term benefits outweigh the risks.
[50] Robertson reported that DBS had been used on 55 adults by 2011, remained an experimental treatment at that time, and recommended that the procedure "should only be conducted by experienced functional neurosurgeons operating in centres which also have a dedicated Tourette syndrome clinic".
[47] Singer (2011) says, "pending determination of patient selection criteria and the outcome of carefully controlled clinical trials, a cautious approach is recommended".
diffusion-weighted imaging based tractography has led to the discovery of the so-called 'depression switch',[54] the intersection of four bundles that allowed more deliberate targeting of DBS in the SCC area and improved results in additional open-label studies.
[57] This target site was discovered serendipitously when a patient with Parkinson's disease developed hypomania under subthalamic nucleus DBS.
[58] While this is not an uncommon side-effect of STN-DBS and alternative pathomechanisms have been suggested,[59][60] the original investigators attributed the occurrence of hypomania to stimulation of a hitherto undescribed 'superolateral' branch of the MFB, which supposedly only exists in humans.
One study[63] of 17 people with intractable cancer pain found that 13 were virtually pain-free and only four required opioid analgesics on release from hospital after the intervention.
[65] Results of DBS in people with dystonia, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases.
[70] In 2015, a group of Brazilian researchers led by neurosurgeon Erich Fonoff [pt] described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS.
Adaptive or closed-loop deep brain stimulation is a technique in which a steering signal influences when, with which amplitude or at which electrode contacts the DBS system is activated.
[80] The potential exists for neuropsychiatric side effects after DBS, including apathy, hallucinations, hypersexuality, cognitive dysfunction, depression, and euphoria.
Medtronic is developing a closed loop system which can be based on automatic feedback and Abbott allows remote programming.