Dental plaque
[1] Interestingly, it has been observed that differences in the composition of dental plaque microbiota exist between men and women, particularly in the presence of periodontitis.
[2] Progression and build-up of dental plaque can give rise to tooth decay – the localised destruction of the tissues of the tooth by acid produced from the bacterial degradation of fermentable sugar – and periodontal problems such as gingivitis and periodontitis;[3] hence it is important to disrupt the mass of bacteria and remove it.
[3] Dental plaque is a biofilm that attaches to tooth surfaces, restorations and prosthetic appliances (including dentures and bridges) if left undisturbed.
The following table provides a more detailed (six-step) explanation of biofilm formation: Different types of bacteria are normally present in the mouth.
These bacteria, as well as leukocytes, neutrophils, macrophages, and lymphocytes, are part of the normal oral cavity and contribute to the individual's health.
[8] The bulk of the microorganisms that form the biofilm are Streptococcus mutans and other anaerobes, though the precise composition varies by location in the mouth.
[1] S. mutans and other anaerobes are the initial colonisers of the tooth surface, and play a major role in the establishment of the early biofilm community.
[9] Streptococcus mutans uses the enzyme glucansucrase to convert sucrose into a sticky, extracellular, dextran-based polysaccharide that allows the bacteria to cohere, forming plaque.
However, failure to remove plaque by regular tooth-brushing allows them to proliferate unchecked and thereby build up in a thick layer, which can by virtue of their ordinary metabolism cause any of various dental diseases for the host.
[15][failed verification] Antibodies to the oral pathogens Campylobacter rectus, Veillonella parvula, Prevotella melaninogenica were associated with hypertension.
[13] The main ecological factors that contribute to plaque formation are pH, saliva, temperature and redox reactions.
[19][20] This indicates that the natural environment of the mouth provided by saliva is ideal for the growth of bacteria in the dental plaque.
[17] In addition to acting as a buffer, saliva and gingival crevicular fluid contain primary nutrients including amino acids, proteins and glycoproteins.
[21] The normal temperature of the mouth ranges between 35 and 36 °C, and a two-degree (°C) change has been shown to drastically shift the dominant species in the plaque.
[22] This is characterized by the cardinal signs of inflammation including a red, puffy appearance of the gums and bleeding due to brushing or flossing.
However, if left for an extended period of time, the inflammation may begin to affect the supporting tissues, in a progression referred to as periodontitis.
This can be treated with strict oral hygiene such as tooth brushing and cleaning in between the teeth as well as surgical debridement completed by a dental professional.
[26] Accumulated bacteria, due to the onset of periodontitis from dental plaque, may gain access to distant sites in the body through the circulatory and respiratory system, potentially contributing to various systematic diseases and conditions.
Saliva is also unable to penetrate the build-up of plaque and thus cannot act to neutralize the acid produced by the bacteria and remineralize the tooth surface.
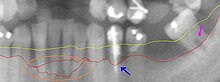
There are two main methods of detecting dental plaque in the oral cavity: through the application of a disclosing gel or tablet, and/or visually through observation.
Before using these at home or in the dental clinic check with your general practitioners for any allergies to iodine, food colouring or any other ingredients that may be present in these products.
These are also helpful educational tools for young children or patients who are struggling to remove dental plaque in certain areas.
[34] Research done by the US National Institute of Health in 2022 studied the antimicrobial properties and effects of a lemongrass essential oil mouthwash.
It showed that after 12 weeks, those who rinsed with the essential oil mouthwash had significantly reduced plaque and improved their gingivitis compared to the groups that only brushed and flossed.
[37] A study involving 20 participants found that mouthwash containing Magnolia grandiflora bark extract performed significantly better than placebo at reducing the prevalence of Streptococcus mutans.
In a 4-year study, a Beagle dog has been put to eat a strict diet without any oral hygiene which led to the accumulation of gingivitis in just a few weeks.
However, some dogs were put on a similar diet with hygiene precautions of daily brushing their teeth and showed no signs of gingivitis.
Some owners express sentiments like "my dog has good teeth for their age," supporting the idea that as animals grow older, their dental features worsen, along with their weight.
[44] It is important to take care of pets by not only keeping them clean and providing them with healthy foods but also maintaining oral cleanliness to avoid discomfort and diseases.