Eumycetoma
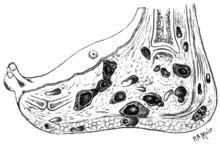
[5] It starts as a painless wet nodule, which may be present for years before ulceration, swelling, grainy discharge and weeping from sinuses and fistulae, followed by bone deformity.
[5] The infection occurs generally in the tropics,[7] and is endemic in Sub-Saharan Africa, especially Sudan, India, parts of South America and Mexico.
[11][12] It appears as a painless wet nodule, which may be present for years before ulceration, swelling and weeping from sinuses, followed by bone deformity.
[13] Black discharge tends to be caused by species from the genera Madurella, Pyrenochaeta, Exophiala, Leptosphaeria and Curvularia.
[21] The disease then spreads to deeper tissues and also forms sinus tracts leading to skin surface.
In the red and yellow varieties deep spread occurs early, infiltrating muscles and bones but sparing nerves and tendons, which are highly resistant to the invasion.
Simple hygienic precautions like wearing shoes or sandals while working in fields, and washing hands and feet at regular intervals may help prevent the disease.
[25] Actinomycetes usually respond well to medical treatment, but eukaryotic infections are generally resistant and may require surgical interventions including salvage procedures as bone resection or even the more radical amputation.
[27][28] The disease is more common in males aged 20–40 years who work as labourers, farmers and herders, and in travellers to tropical regions, where the condition is endemic.
[12] The first modern description of Madura foot was made in 1842 from Madurai (the city after which the disease was named Madura-mycosis) in India, by Gill.
[7] Traditionally occurring in regions where resources are scarce, medicines may be expensive and diagnosis is frequently made late, when more invasive treatment may be required.