Gingival and periodontal pocket
[2] The gingival tissue forms a crevice surrounding the tooth, similar to a miniature, fluid-filled moat, wherein food debris, endogenous and exogenous cells, and chemicals float.
The depth of this crevice, known as a sulcus, is in a constant state of flux due to microbial invasion and subsequent immune response.
This early sign of disease in the mouth is completely reversible when the etiology of the edematous reaction is eliminated and frequently occurs without dental surgical therapy.
[6] Plaque that has been present long enough to harden and calcify will welcome additional bacteria to the pocket and make it virtually impossible to clean by means of a traditional toothbrush.
[7] Continuous destruction of surrounding tissues due to inflammation will lead to degradation of attachment and bone, eventually causing tooth loss.
These can either be systemic (like diabetes or smoking) or local (like overhanging dental restorative materials causing food trap).
Early detection of high plaque levels at routine dental visits are found to be beneficial to avoid progression of the pocket formation.
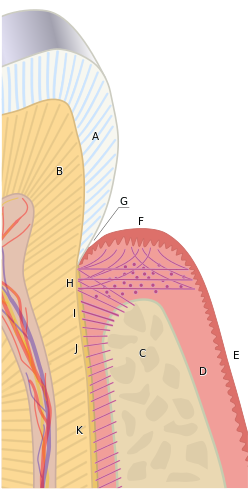
B) Root of the tooth, covered by cementum
C) Alveolar bone
D) Subepithelial connective tissue
E) Oral epithelium
F) Free gingival margin
G) Gingival sulcus (extensions of which are the gingival and periodontal pockets )
H) Principal gingival fibers
I) Alveolar crest fibers of the periodontal ligament (PDL)
J) Horizontal fibers of the PDL
K) Oblique fibers of the PDL
