Granulomatosis with polyangiitis
[6] The signs and symptoms of GPA are highly varied and reflect which organs are supplied by the affected blood vessels.
Typical signs and symptoms include nosebleeds, stuffy nose and crustiness of nasal secretions, and inflammation of the uveal layer of the eye.
[3] GPA is rare in Japanese and African-American populations but occurs more often in people of Northern European descent.
[11] Initial signs are highly variable, and diagnosis can be severely delayed due to the nonspecific nature of the symptoms.
[13][18] Classic microscopic features of GPA include inflammation of blood vessels associated with poorly formed granulomas, necrosis, and many giant cells.
[7] In vitro studies have found that ANCAs can activate neutrophils, increase their adherence to endothelium, and induce their degranulation that can damage endothelial cells.
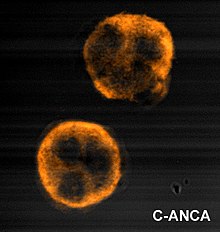
[19] Cytoplasmic-staining ANCAs that react with the enzyme proteinase 3 (cANCA) in neutrophils (a type of white blood cells) are associated with GPA.
On histopathological examination, a biopsy will show leukocytoclastic vasculitis with necrotic changes and granulomatous inflammation (clumps of typically arranged white blood cells) on microscopy.
[12] Granulomatosis with polyangiitis is part of a larger group of vasculitic syndromes called systemic vasculitides or necrotizing vasculopathies, all of which feature an autoimmune attack by an abnormal type of circulating antibody termed ANCAs (antineutrophil cytoplasmic antibodies) against small and medium-sized blood vessels.
[1] Although GPA affects small- and medium-sized vessels,[20] it is formally classified as one of the small-vessel vasculitides in the Chapel Hill system.
[8] The standard treatment for severe GPA is to induce remission with immunosuppressants such as rituximab or cyclophosphamide in combination with high-dose corticosteroids.
[8][25] Plasmapheresis is sometimes recommended for very severe manifestations of GPA, such as diffuse alveolar hemorrhage and rapidly progressive glomerulonephritis (as seen in pulmonary-renal syndrome).
[8] Due to a high frequency of abnormally low white blood cell counts seen with cyclophosphamide treatment, Pneumocystis jirovecii pneumonia is a common complication, so prophylaxis against this pathogen is recommended.
[25][26] The dose of corticosteroids is generally tapered (decreased) very slowly over several months to reduce the risk of another GPA flare.
[13] Long-term complications are common (86%), mainly chronic kidney failure, hearing loss, and deafness.
[31] Scottish otolaryngologist Peter McBride (1854–1946) first described the condition in 1897 in a British Medical Journal article entitled "Photographs of a case of rapid destruction of the nose and face".