Goodpasture syndrome
Due to the GPS's rapid progression, the significant difficulty of treating the disease is identifying it early and making the appropriate response before severe damage occurs to the kidneys and or lungs.
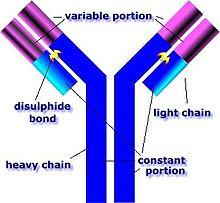
[5][6] The anti–glomerular basement membrane (GBM) antibodies primarily attack the kidneys and lungs, although, generalized symptoms like malaise, weight loss, fatigue, fever, and chills are also common, as are joint aches and pains.
[8] Some other signs and symptoms that could be used to identify Goodpasture syndrome during a physical exam include an increased respiratory rate, cyanosis, crackles, hepatosplenomegaly, and hypertension.
[10] In addition to genetic susceptibility, an initial environmental insult to the pulmonary vasculature is needed to allow the anti-glomerular basement membrane (anti-GBM) antibodies to reach the alveolar capillaries.
[11] The major target of these abnormal antibodies is the non-collagen domain of the alpha-3 chain of type 4 collagen, which is mostly found in the basal membranes of glomerular and alveolar capillaries, explaining the obscurely specific symptoms of this condition.
[11] In addition, if there is substantial suspicion of the disease, serologic testing for ELISA assay is usually done by looking for alpha3 NC1 domain area of collagen IV in order to avoid false positives.
[18] The major mainstay of treatment for GPS is plasmapheresis, a procedure in which the affected person's blood is sent through a centrifuge and the various components separated based on weight.
[11] A study performed in Australia and New Zealand demonstrated that in patients requiring renal replacement therapy (including dialysis) the median survival time is 5.93 years.