Gut–brain axis
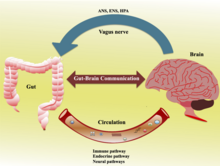
[5] The bidirectional communication is done by immune, endocrine, humoral and neural connections between the gastrointestinal tract and the central nervous system.
Studies have confirmed that gut microbiome contribute to range of brain functions controlled by the hippocampus, prefrontal cortex and amygdala (responsible for emotions and motivation) and act as a key node in the gut-brain behavioral axis.
[9] While Irritable bowel syndrome (IBS) is the only disease confirmed to be directly influenced by the gut microbiome, many disorders (such as anxiety, autism, depression and schizophrenia) have been reportedly linked to the gut-brain axis as well.
[6][10][7] According to a study from 2017, "probiotics have the ability to restore normal microbial balance, and therefore have a potential role in the treatment and prevention of anxiety and depression".
[11] The first of the brain–gut interactions shown, was the cephalic phase of digestion, in the release of gastric and pancreatic secretions in response to sensory signals, such as the smell and sight of food.
The enteric nervous system also makes use of more than 30 neurotransmitters, most of which are identical to the ones found in CNS, such as acetylcholine, dopamine, and serotonin.
[25] In humans, the gut microbiota has the largest quantity of bacteria and the greatest number of species, compared to other areas of the body.
[25] Human gut microorganisms benefit the host by collecting the energy from the fermentation of undigested carbohydrates and the subsequent absorption of short-chain fatty acids (SCFAs), acetate, butyrate, and propionate.
[citation needed] Additional health factors that may skew the composition of the gut microbiota are antibiotics and probiotics.
[32] Changes in the composition of the gut microbiota due to diet, drugs, or disease correlate with changes in levels of circulating cytokines, some of which can affect brain function.
[32] The gut microbiota also release molecules that can directly activate the vagus nerve, which transmits information about the state of the intestines to the brain.
[32] Likewise, chronic or acutely stressful situations activate the hypothalamic–pituitary–adrenal axis, causing changes in the gut microbiota and intestinal epithelium, and possibly having systemic effects.
[32] Most of the work that has been done on the role of gut microbiota in the gut–brain axis has been conducted in animals, including the highly artificial germ-free mice.
As of 2016, studies with humans measuring changes to gut microbiota in response to stress, or measuring effects of various probiotics, have generally been small and cannot be generalized; whether changes to gut microbiota are a result of disease, a cause of disease, or both in any number of possible feedback loops in the gut–brain axis, remains unclear.
[35] While Irritable bowel syndrome (IBS) is the only disease confirmed to be directly influenced by the gut microbiome, many disorders such as anxiety, autism, depression and schizophrenia have been linked to the gut-brain axis as well.
[6][36][7] Skin conditions such as acne were proposed as early as 1930,[37] to be related to emotional states which altered the gut microbiome leading to systemic inflammation.
[40] Brain function is dependent on multiple neuropeptides including dopamine, GABA and serotonin, that are controlled in the gut microbiota.
[44] Braak's theory proposed that gut dysbiosis in Parkinson's causes the aggregation of alpha-synuclein in the gastrointestinal tract before its spreading to the brain.
Relevant therapies are the Vagus nerve stimulation, the Fecal microbiota transplantation, the use of Rifaximun and other drugs directed towards the gut.