Health
For a long time, it was set aside as an impractical ideal, with most discussions of health returning to the practicality of the biomedical model.
In 1984, WHO revised the definition of health defined it as "the extent to which an individual or group is able to realize aspirations and satisfy needs and to change or cope with the environment.
Mental, intellectual, emotional and social health referred to a person's ability to handle stress, to acquire skills, to maintain relationships, all of which form resources for resiliency and independent living.
Since the late 1970s, the federal Healthy People Program has been a visible component of the United States' approach to improving population health.
[6] In each decade, a new version of Healthy People is issued,[7] featuring updated goals and identifying topic areas and quantifiable objectives for health improvement during the succeeding ten years, with assessment at that point of progress or lack thereof.
Progress has been limited to many objectives, leading to concerns about the effectiveness of Healthy People in shaping outcomes in the context of a decentralized and uncoordinated US health system.
Genetics, or inherited traits from parents, also play a role in determining the health status of individuals and populations.
This can encompass both the predisposition to certain diseases and health conditions, as well as the habits and behaviors individuals develop through the lifestyle of their families.
For example, genetics may play a role in the manner in which people cope with stress, either mental, emotional or physical.
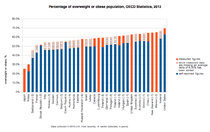
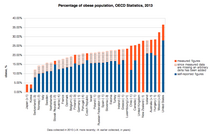
For example, obesity is a significant problem in the United States that contributes to poor mental health and causes stress in the lives of many people.
[28] Among communicable diseases, both viral and bacterial, AIDS/HIV, tuberculosis, and malaria are the most common, causing millions of deaths every year.
Approximately 7.5 million children under the age of 5 die from malnutrition, usually brought on by not having the money to find or make food.
Inactivity can also contribute to health issues and also a lack of sleep, excessive alcohol consumption, and neglect of oral hygiene.
Nutrients help build and strengthen bones, muscles, and tendons and also regulate body processes (i.e., blood pressure).
[46] The CDC states that physical exercise can reduce the risks of heart disease, cancer, type 2 diabetes, high blood pressure, obesity, depression, and anxiety.
Participating in any exercising, whether it is housework, yardwork, walking or standing up when talking on the phone, is often thought to be better than none when it comes to health.
Legal, credentialing and financing frameworks are established by individual governments, augmented on occasion by international organizations, such as churches.
From ancient times, Christian emphasis on practical charity gave rise to the development of systematic nursing and hospitals and the Catholic Church today remains the largest non-government provider of medical services in the world.
Access to information on conditions, treatments, quality, and pricing greatly affects the choice by patients/consumers and, therefore, the incentives of medical professionals.
There is a perceived tension between the need for transparency on the one hand and such issues as patient confidentiality and the possible exploitation of information for commercial gain on the other.
These include treatment of acute and chronic illnesses, preventive care and health education for all ages and both sexes.
The population in question can be as small as a handful of people or as large as all the inhabitants of several continents (for instance, in the case of a pandemic).
Its aim is to prevent health problems from happening or re-occurring by implementing educational programs, developing policies, administering services and conducting research.
One issue is the access of individuals and communities to health care in terms of financial, geographical or socio-cultural constraints.
These include personal actions for preventing or minimizing the effects of a disease, usually a chronic condition, through integrative care.
They also include personal hygiene practices to prevent infection and illness, such as bathing and washing hands with soap; brushing and flossing teeth; storing, preparing and handling food safely; and many others.
The information gleaned from personal observations of daily living – such as about sleep patterns, exercise behavior, nutritional intake and environmental features – may be used to inform personal decisions and actions (e.g., "I feel tired in the morning so I am going to try sleeping on a different pillow"), as well as clinical decisions and treatment plans (e.g., a patient who notices his or her shoes are tighter than usual may be having exacerbation of left-sided heart failure, and may require diuretic medication to reduce fluid overload).
[70] Prolonged psychological stress may negatively impact health, and has been cited as a factor in cognitive impairment with aging, depressive illness, and expression of disease.
Psychological methods include cognitive therapy, meditation, and positive thinking, which work by reducing response to stress.
Contemporary problems, such as the growing rate of obesity and issues relating to stress and overwork in many countries, have further complicated the interaction between work and health.