Diagnosis of HIV/AIDS
Nonspecific reactions, hypergammaglobulinemia, or the presence of antibodies directed to other infectious agents that may be antigenically similar to HIV can produce false positive results.
The World Health Organization estimated that, as of 2000[update], inadequate blood screening had resulted in 1 million new HIV infections worldwide.
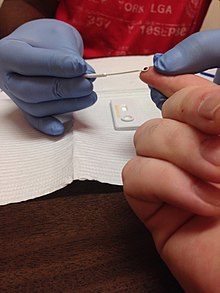
[citation needed] In developing countries, home-based HIV testing and counseling (HBHTC) is an emerging approach for addressing confidentiality issues.
HBHTC allows individuals, couples, and families to learn their HIV status in the convenience and privacy of their home environment.
[9] In 2006, the Centers for Disease Control (CDC) announced an initiative for voluntary, routine testing of all Americans aged 13–64 during health care encounters.
[10] The CDC recommends elimination of requirements for written consent or extensive pre-test counseling as barriers to widespread routine testing.
[10] In 2006, the National Association of Community Health Centers implemented a model for offering free, rapid HIV testing to all patients between the ages of 13 and 64 during routine primary medical and dental care visits.
[11] In September 2010, New York became the first state to require that hospitals and primary care providers offer an HIV test to all patients between the ages of 13 and 64 years.
Those patients must take ELISA tests at various intervals after the usual 28-day course of treatment, sometimes extending outside of the conservative window period of 6 months.
The enzyme-linked immunosorbent assay (ELISA), or enzyme immunoassay (EIA), was the first screening test commonly employed for HIV.
It is compatible to any smartphone or computer without additional support or battery power, and takes some fifteen minutes to analyse a drop of blood.
[citation needed] Specifically, cells that may be HIV-infected are opened and the proteins within are placed into a slab of gel, to which an electric current is applied.
Different proteins will move with different speeds in this field, depending on their size, while their electrical charge is leveled by a surfactant called sodium lauryl sulfate.
[citation needed] There are no universal criteria for interpreting the western blot test: The number of viral bands that must be present may vary.
[citation needed] The ELISA antibody tests were developed to provide a high level of confidence that donated blood was not infected with HIV.
[citation needed] Rare false positive results due to factors unrelated to HIV exposure are found more often with the ELISA test than with the western blot.
When the ELISA test is combined with Western Blot, the rate of false positives is extremely low, and diagnostic accuracy is very high (see below).
The evidence regarding the risks and benefits of HIV screening was reviewed in July 2005 by the U.S. Preventive Services Task Force.
[19] The authors concluded that: ...the use of repeatedly reactive enzyme immunoassay followed by confirmatory western blot or immunofluorescent assay remains the standard method for diagnosing HIV-1 infection.
[citation needed] In blood donation screening, this test is no longer used routinely in the US[28] or the EU[29] since the objective was to reduce the risk of false negatives in the window period.
The presence of p24 antigen diminishes as the body increases production of antibodies to the p24 protein, making p24 more difficult to detect later.
Although this results in a dramatic decrease in cost, the dilution of the virus in the pooled samples decreases the effective sensitivity of the test, lengthening the window period by four days (assuming a 20-fold dilution, ~20hr virus doubling time, detection limit 50 copies/ml, making limit of detection 1,000 copies/ml).
[34] A different version of this test is intended for use in conjunction with clinical presentation and other laboratory markers of disease progress for the management of HIV-1-infected patients.
[citation needed] In the Quantiplex bDNA or branched DNA test, plasma is placed in a centrifuge to concentrate the virus, which is then opened to release its RNA.
Monitoring the effects of antiretroviral therapy by serial measurements of plasma HIV-1 RNA with this test has been validated for patients with viral loads greater than 25,000 copies per milliliter.
[35] The South African government announced a plan to start screening for HIV in secondary schools by March 2011.
[citation needed] This test is also used occasionally to estimate immune system function for people whose CD4 T cells are impaired for reasons other than HIV infection, which include several blood diseases, several genetic disorders, and the side effects of many chemotherapy drugs.
[39] Despite the increase in false positives in NYC DOHMH, the CDC still continues to support the use of noninvasive oral fluid specimens due to their popularity in health clinics and convenience of use.
The director of the HIV control program for public health at Seattle King county, reported OraQuick failed to spot at least 8 percent of 133 people found to be infected with a comparable diagnostic test.
In 1997, a California man was indicted on mail fraud and wire charges for selling supposed home test kits.