HPV-positive oropharyngeal cancer
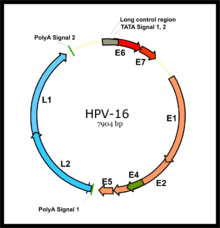
Efforts are being made to reduce the incidence of HPV-positive OPC by introducing vaccination that includes HPV types 16 and 18, found in 95% of these cancers, before exposure to the virus.
In the past, the treatment of OPC was radical surgery, with an approach through the neck and splitting of the jaw bone, which resulted in morbidity and poor survival rates.
In the absence of high-quality evidence regarding which treatment provides the best outcomes, management decisions are often based on one or more of the following: technical factors, likely functional loss, and patient preference.
HPV+OPC presents in one of four ways: as an asymptomatic abnormality in the mouth found by the patient or a health professional such as a dentist; with local symptoms such as pain or infection at the site of the tumor; with difficulties of speech, swallowing, and/or breathing; or as a swelling in the neck (if the cancer has spread to lymph nodes).
[10][11][12] Human HPV has long been implicated in the pathogenesis of several anogenital cancers including those of the anus, vulva, vagina, cervix, and penis.
The naturally occurring (wild type) p53 is widely involved in cellular processes, including autophagy, response to DNA damage, cell cycle regulation, and senescence, apoptosis and the generation of adenosine triphosphate (ATP) through oxidative phosphorylation.
[46][47][11] The tonsillar epithelia (palatine and lingual) share similar nonkeratinization characteristics with the cervix, where HPV infection plays the major role in cases of cervical cancer.
This, in turn, could restrict the malignant behaviour of HPV+OPC and the presence of antibodies has been associated with a better prognosis, while treatment may enhance the immunogenicity of the tumour, and hence improve response, although to what extent is not clear.
[14] There is not a standard HPV testing method in head and neck cancers,[63] both in situ hybridization (ISH) and polymerase chain reaction (PCR) are commonly used.
[65] Immunohistochemistry (IHC) staining of the tissue for p16 is frequently used as a cost-effective surrogate for HPV in OPC, compared to ISH or PCR[66][67][68] but there is a small incidence of HPV-negative p16-positive disease accounting for about 5% of HPV-OPC.
[69] HPV+OPC has been treated similarly to stage-matched and site-matched HPV-unrelated OPC, but its unique features, which contrast smoking-related HPV-OPC head and neck cancers, for which patients' demographics, comorbidities, risk factors, and carcinogenesis differ markedly, suggest that a distinct staging system be developed to more appropriately represent the severity of the disease and its prognosis.
Consequently, less intensive (de-intensification) use of radiotherapy or chemotherapy,[77] as well as specific therapy, is under investigation, enrolling HPV+OPC in clinical trials to preserve disease control and minimise morbidity in selected groups based on modified TNM staging and smoking status.
[85] The goals of treatment are to optimise survival and locoregional disease control, and prevent spread to distant areas of the body (metastasis), while minimising short- and long-term morbidity.
[11] Furthermore, it is suggested that the effects of E6 and E7 on these pathways render the tumour more radiosensitive, possibly by interference with mechanisms such as DNA repair, repopulation signalling, and cell-cycle redistribution.
Surgical management of OPC carried significant morbidity with a transcervical (through the neck) approach, often involving mandibulotomy, in which the jawbone (mandible) is split.
For tumours of the tonsil and lateral pharyngeal wall, and clinically node-negative (N0) disease, dissection of the neck typically involves levels 2–4 (see diagram in Dubner 2017) ipsilaterally.
[12] An advantage of a primary surgical approach is the amount of pathological information made available, including grade, margin status, and degree of involvement of lymph nodes.
Subsequently, there was a tendency to intensify treatment in head and neck cancer, and many centres adopted a dose of 66 Gy, at least for those patients with adverse tumour features.
[126] In one single institution study, a decision was made to reduce the radiation dose in high-risk patients with HPV+OPC from 66 to 60 Gy, corresponding to the actual evidence, and follow-up has shown no decrease in cancer control.
[136][137] Reported toxicities include dry mouth (xerostomia) from salivary gland damage, 18% (grade 2);[f] difficulty swallowing (dysphagia) from damage to the constrictor muscles, larynx and oesophageal sphincter, 15% (grade 2); subclinical aspiration up to 50% (reported incidence of aspiration pneumonia approximately 14%); hypothyroidism 28–38% at three years (may be up to 55% depending on amount of the thyroid gland exposed to over 45 Gy radiation; esophageal stenosis 5%; osteonecrosis of the mandible 2.5%; and need for a gastrostomy tube to be placed at some point during or up to one year after treatment 4% (up to 16% with longer follow up).
[12] Concerns have been expressed regarding excessive short- and long-term toxicity, especially dysphagia and xerostomia,[142][143][144] and hence whether standard doses expose patients with better prognoses to overtreatment and unnecessary side effects.
[166] Ongoing studies, following the experience of the Mayo Clinic trial (MC1273),[130] such as that the Memorial Sloan Kettering Cancer Center are exploring doses as low as 30Gy.
[144] Although chemoradiation became a treatment standard based on clinical trials and in particular, meta-analyses, a subsequent population-based study of patients with OPC, indicated no advantage to the addition of chemotherapy to radiation in either HPV+OPC or HPV-OPC,[173] and significant concerns about added toxicity.
[175] Generally it is used where the pathology of the resected specimen indicates features associated with a high risk of locoregional recurrence (e.g. extracapsular extension through involved lymph nodes or very close margins).
In the GORTEC trial, chemotherapy with docetaxel provided improved survival and locoregional control in locally advanced OPC but was associated with increased mucositis and need for feeding by gastrostomy.
[191][192][193] Early stage disease[q] is associated with a relatively favourable outcome, for which single modality therapy is recommended, the choice depending on tumour location and accessibility.
[197] In the absence of specific clinical trials and guidelines, patient preferences need to be taken into consideration to minimise short- and long-term toxicity and functional loss and optimize quality of life, given the prolonged survival frequently seen.
[204] Tumor HPV status is strongly associated with positive therapeutic response and survival compared with HPV-negative cancer, independent of the treatment modality chosen and even after adjustment for the stage.
[217] Less detailed information is available for those treated primarily with surgery, for whom fewer patients are available,[122] as well as low rates of recurrence (7–10%), but features that have traditionally been useful in predicting prognosis in other head and neck cancers, appear to be less useful in HPV+OPC.
[30] A possible explanation for the favourable impact of HPV+ is "the lower probability of occurrence of 11q13 gene amplification, which is considered to be a factor underlying faster and more frequent recurrence of the disease"[14] Presence of TP53 mutations, a marker for HPV- OPC, is associated with worse prognosis.