Healthcare industry
It can be further subdivided into numerous sectors and categories and relies on interdisciplinary teams of highly skilled professionals and paraprofessionals to address the healthcare requirements of both individuals and communities.
[3] Consuming over 10 percent of gross domestic product (GDP) of most developed nations, health care can form an enormous part of a country's economy.
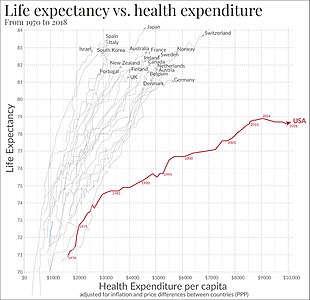
[4] The per capita expenditure on health and pharmaceuticals in OECD countries has steadily grown from a couple of hundred in the 1970s to an average of US$4'000 per year in current purchasing power parities.
The latter listed industry group includes companies that produce biotechnology, pharmaceuticals, and miscellaneous scientific services.
[6] A healthcare provider is an institution (such as a hospital or clinic) or person (such as a physician, nurse, allied health professional or community health worker) that provides preventive, curative, promotional, rehabilitative or palliative care services in a systematic way to individuals, families or communities.
The incomes of managers and administrators, underwriters, and medical malpractice attorneys, marketers, investors, and shareholders of for-profit services, all are attributable to health care costs.
[8] In 2017, healthcare costs paid to hospitals, physicians, nursing homes, diagnostic laboratories, pharmacies, medical device manufacturers, and other components of the healthcare system, consumed 17.9 percent of the gross domestic product (GDP) of the United States, the largest of any country in the world.
Health protection is costly and hospital expenses are overwhelmingly the most well-known explanation behind individual liquidation in the United States.
In many poorer countries, development aid, as well as funding through charities or volunteers, help support the delivery and financing of health care services among large segments of the population.
Over the first twenty-five years of this transformation, government contributions to healthcare expenditures have dropped from 36% to 15%, with the burden of managing this decrease falling largely on patients.
The system is the guiding basis of the modern British healthcare model enacted post-World War II.
However, depending on the specific system, public providers can be accompanied by private doctors who collect fees from the government.
The system attempts to cover all working citizens, meaning patients cannot be excluded from insurance due to pre-existing conditions.
The emergence of the National Health Insurance model is cited as a response to the challenges presented by the traditional Bismarck and Beveridge systems.
However, large public insurance programs provide the government with bargaining power, allowing them to drive down prices for certain services and medication.
[28] In areas with low levels of government stability or poverty, there is often no mechanism for ensuring that health costs are covered by a party other than the individual.
[29] The UK National Health System creates excellent patient outcomes and mandates universal coverage but also has large lag times for treatment.
Critics argue that reforms brought about by the Health and Social Care Act 2012 only proved to fragment the system, leading to high regulatory burden and long treatment delays.