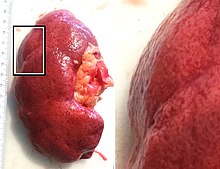
Hypertensive kidney disease
Additional complications often associated with hypertensive nephropathy include glomerular damage resulting in protein and blood in the urine.
This leads to a build-up of plaques and they can be deposited in the renal arteries causing stenosis and ischemic kidney disease.
Other consequences include arterial stiffening, which involves a gradual breakdown of elastic fibers and intima (the innermost layer of a blood vessel) thickening.
[10] The large renal arteries exhibit intimal thickening, medial hypertrophy, duplication of the elastic layer.
The changes in small arterioles include hyaline arteriolosclerosis (deposition of hyaline, collagenous material),[citation needed] which causes glomerular collapse (wrinkling and thickening of capillary basement membranes and collapse of capillary lumen) and solidification (glomeruli exhibit sclerosis and increase in mesangial matrix).
[11] Vessels feature intimal thickening, fibrinoid necrosis, red blood cell fragmentation, extravasation, thrombosis.
[citation needed] Increasing access to, and use of, genome profiling may provide opportunity for diagnosis based on presentation and genetic risk factors, by identifying ApoL1 gene variants on chromosome 22.
[13] The aim of the medical treatment is to slow the progression of chronic kidney disease by reducing blood pressure and albumin levels.
[14] The current published guidelines define ideal BP of <130/80 mmHg for patients with hypertensive nephropathy; studies show that anything higher or lower than this can increase cardiovascular risk.
The management plan should be individualized based on the condition of the patients including comorbidities and previous medical history.
Patient prognosis is dependent on numerous factors including age, ethnicity, blood pressure and glomerular filtration rate.
Changes in lifestyle factors, such as reduced salt intake and increased physical activity have been shown to improve outcomes but are insufficient without pharmacological treatment.
In addition to this, African Americans tend to develop hypertensive nephropathy at a younger age than Caucasians (45 to 65, compared to >65).