Cirrhosis
[13] As the disease worsens, symptoms may include itchiness, swelling in the lower legs, fluid build-up in the abdomen, jaundice, bruising easily, and the development of spider-like blood vessels in the skin.
[1] More serious complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus, stomach, or intestines, and liver cancer.
[20] MASH has several causes, including obesity, high blood pressure, abnormal levels of cholesterol, type 2 diabetes, and metabolic syndrome.
[21] Less common causes of cirrhosis include autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis that disrupts bile duct function, genetic disorders such as Wilson's disease and hereditary hemochromatosis, and chronic heart failure with liver congestion.
[1] No specific treatment for cirrhosis is known, but many of the underlying causes may be treated by medications that may slow or prevent worsening of the condition.
[21] Biannual screening for liver cancer using abdominal ultrasound, possibly with additional blood tests, is recommended[22][23] due to the high risk of hepatocellular carcinoma arising from dysplastic nodules.
[25] The term "cirrhosis" was derived in 1819 from the Greek word "kirrhos", which describes the yellowish color of a diseased liver.
[13] As cirrhosis progresses, symptoms may include neurological changes affecting both the peripheral and central nervous systems, disrupting the neurotransmission within the brain and causing neuromuscular fatigue.
[28] Worsening cirrhosis can cause a build-up of fluid in different parts of the body such as the legs (edema) and abdomen (ascites).
[49][33] The liver plays a vital role in many metabolic processes in the body including protein synthesis, detoxification, nutrient storage (such as glycogen), platelet production and clearance of bilirubin.
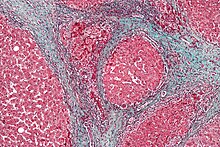
Damage to the liver tissue from inflammation leads to the activation of stellate cells, which increases fibrosis through the production of myofibroblasts, and obstructs hepatic blood flow.
[60] In addition, stellate cells secrete TGF beta 1, which leads to a fibrotic response and proliferation of connective tissue.
TGF-β1 have been implicated in the process of activating hepatic stellate cells (HSCs) with the magnitude of fibrosis being in proportion to increase in TGF β levels.
[62][63] As this cascade of processes continues, fibrous tissue bands (septa) separate hepatocyte nodules, which eventually replace the entire liver architecture, leading to decreased blood flow throughout.
[45] Portable ultrasound is a low cost tool to identify the sign of liver surface nodularity with a good diagnostic accuracy.
[109] The variables include all Model for End-Stage Liver Disease (MELD)'s components, as well as sodium, albumin, total cholesterol, white blood cell count, age, and length of stay.
Key prevention strategies for cirrhosis are population-wide interventions to reduce alcohol intake (through pricing strategies, public health campaigns, and personal counseling), programs to reduce the transmission of viral hepatitis, and screening of relatives of people with hereditary liver diseases.
There is no evidence that supports the avoidance or dose reduction of paracetamol in people with compensated cirrhosis; it is thus considered a safe analgesic for said individuals.
Similarly, control of weight and diabetes prevents deterioration in cirrhosis due to non-alcoholic fatty liver disease.
In patients with previously stable cirrhosis, decompensation may occur due to various causes, such as constipation, infection (of any source), increased alcohol intake, medication, bleeding from esophageal varices or dehydration.
People with decompensated cirrhosis generally require admission to a hospital, with close monitoring of the fluid balance, mental status, and emphasis on adequate nutrition and medical treatment – often with diuretics, antibiotics, laxatives or enemas, thiamine and occasionally steroids, acetylcysteine and pentoxifylline.
[126] Administration of saline is avoided, as it would add to the already high total body sodium content that typically occurs in cirrhosis.
Clotting function is estimated by lab values, mainly platelet count, prothrombin time (PT), and international normalized ratio (INR).
The American Gastroenterological Association (AGA) provided recommendations in 2021 in regards to coagulopathy management of cirrhotic patients in certain scenarios.
[140] Per 2014 guidelines,[141] the first-line treatment involves the use of lactulose, a non-absorbable disaccharide which decreases the pH level of the colon when it is metabolized by intestinal bacteria.
[142] Rifaximin, an antibiotic that inhibits the function of ammonia-producing bacteria in the gastrointestinal tract,[143] is recommended for use in combination with lactulose as prophylaxis against recurrent episodes of hepatic encephalopathy.
[146] Several factors may precipitate hepatic encephalopathy, which include alcohol use, excess protein, gastrointestinal bleeding, infection, constipation, and vomiting/diarrhea.
[150] Moreover, infections in cirrhosis are major triggers for other complications (ascites, variceal bleeding, hepatic encephalopathy, organ failures, death).
[156] Cirrhosis and chronic liver disease were the tenth leading cause of death for men and the twelfth for women in the United States in 2001, killing about 27,000 people each year.
[159] The word "cirrhosis" is a neologism derived from Greek: κίρρωσις; kirrhos κιρρός, meaning "yellowish, tawny" (the orange yellow colour of the diseased liver) and the suffix -osis, i.e. "condition" in medical terminology.