Liver tumor
They may be discovered on medical imaging (even for a different reason than the cancer itself), and the diagnosis is often confirmed with liver biopsy.
They are caused by either abnormal growth of neoplastic cells or in response to liver injury, known as regenerative nodules.
[2][5] Cavernous hemangiomas are diagnosed with medical imaging (do not usually need biopsy to confirm diagnosis).
[2] Given their benign course and often asymptomatic nature, cavernous hemangiomas are typically diagnosed incidentally (e.g. when medical imaging is obtained for another reason).
[5] If the cavernous hemangioma grows quickly or the patient is symptomatic, further medical intervention is warranted.
[5] Therapies include open or laparoscopic surgical resection, arterial embolization, or radio-frequency ablation.
[2] It is common for patients to have multiple distinct liver lesions; however, they do not tend to grow over time and they do not typically convert to malignant tumors.
[2] The majority of FNH have a characteristic "central scar" on contrast-enhanced imaging, which helps to solidify the diagnosis.
[2] However, if a central scar is not present on imaging, it is hard to tell the difference between FNH, hepatic adenoma, and hepatocellular carcinoma, in which cases biopsy is the next step to aid in the diagnosis process.
[7] They are also associated with glycogen storage diseases (subtypes I and III), and newer studies are suggesting that diabetes, obesity, high blood pressure, and dyslipidemia are risk factors for hepatic adenomas.
[7] However, if signs and symptoms are present they include non-specific abdominal pain, yellowing of skin, and higher than normal gamma glutamyl transferase and alkaline phosphatase laboratory values.
[7] Molecular categorization via biopsy and pathological analysis aids in both diagnosis and understanding prognosis, particularly because hepatocellular adenomas have the potential to become malignant.
[2][7] It is important to note, percutaneous biopsy should be avoided, because this method can lead to bleeding or rupture of the adenoma.
[2] Currently, if the hepatic adenoma is >5 cm, increasing in size, symptomatic lesions, has molecular markers associated with HCC transformation, rising level of liver tumor markers such as alpha fetoprotein, the patient is a male, or has a glycogen storage disorder, the adenoma is recommended to be surgically removed.
These include sonography (ultrasound), computed tomography (CT) and magnetic resonance imaging (MRI).
High levels of alpha-fetoprotein (AFP) in the blood can be found in many cases of HCC and intrahepatic cholangiocarcinoma.
Tumor characterization using the ultrasound method will be based on the following elements: consistency (solid, liquid, mixed), echogenicity, structure appearance (homogeneous or heterogeneous), delineation from adjacent liver parenchyma (capsular, imprecise), elasticity, posterior acoustic enhancement effect, the relation with neighboring organs or structures (displacement, invasion), vasculature (presence and characteristics on Doppler ultrasonography and contrast-enhanced ultrasound (CEUS).
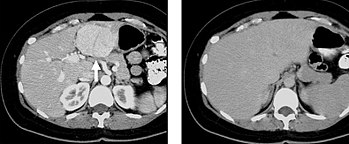
[citation needed] When evaluating hepatic masses by abdominal computed tomography (CT), it can be advantageous to have both late arterial and portal venous phase images since some tumors enhance briskly during the arterial phase (hepatocellular carcinoma, hepatic adenoma, follicular nodular hyperplasia (FNH), and hypervascular metastasis), but maybe occult or difficult to characterize on portal venous phase imaging alone.
In addition, if there is a need to definitively characterize a hepatic mass, MRI is generally more sensitive and specific, with no associated radiation dose.