Luteinizing hormone
In males, where LH had also been called interstitial cell–stimulating hormone (ICSH),[5] it stimulates Leydig cell production of testosterone.
[6] This is in reference to the corpus luteum, which is a mass of cells that forms in an ovary after an ovum (egg) has been discharged.
Each monomeric unit is a glycoprotein molecule; one alpha and one beta subunit make the full, functional protein.
LH supports theca cells in the ovaries that provide androgens and hormonal precursors for estradiol production.
At the time of menstruation, FSH initiates follicular growth, specifically affecting granulosa cells.
[16] Some studies, however, attribute the LH surge to positive feedback from estradiol after production by the dominant follicle exceeds a certain threshold.
Exceptionally high levels of estradiol induce hypothalamic production of progesterone, which stimulates elevated GnRH secretion, triggering a surge in LH.
Gonadal steroids (estrogens and androgens) generally have negative feedback effects on GnRH-1 release at the level of the hypothalamus and at the gonadotropes, reducing their sensitivity to GnRH.
Positive feedback by estrogens also occurs in the gonadal axis of female mammals and is responsible for the midcycle surge of LH that stimulates ovulation.
As estrogens' levels gradually increase the positive effect predominates, leading to the LH surge.
Binding to this receptor causes an increase in cyclic adenosine monophosphate (cAMP), a secondary messenger, which allows cholesterol to translocate into the mitochondria.
[19] As the levels of testosterone increase, it will act on the pituitary through a negative feedback loop and inhibit the release of GnRH and LH consequently.
[24] Androgens (including testosterone and dihydrotestosterone) inhibit monoamine oxidase (MAO) in the pineal gland, leading to increased melatonin and reduced LH and FSH by melatonin-induced increase of Gonadotropin-Inhibitory Hormone (GnIH)[25] synthesis and secretion.
[26] Changes in LH and testosterone blood levels and pulse secretions are induced by changes in sexual arousal in human males.
Since LH is secreted as pulses, it is necessary to follow its concentration over a sufficient period of time to get proper information about its blood level.
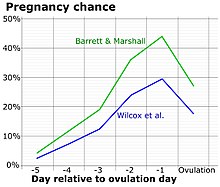
[36] A conversion from a negative to a positive reading would suggest that ovulation is about to occur within 24–48 hours, giving women two days to engage in sexual intercourse or artificial insemination with the intention of conceiving.
For example, the Clearblue test is taken daily, and an increased frequency does not decrease the risk of missing an LH surge.
Steroidogenesis entails processes by which cholesterol is converted to biologically active steroid hormones.
A study shows that LH via a PKA signaling pathway regulates the phosphorylation and localization of DRP1 within mitochondria of the steroidogenic cells of the ovary.


- The ranges denoted By biological stage may be used in closely monitored menstrual cycles in regard to other markers of its biological progression, with the time scale being compressed or stretched to how much faster or slower, respectively, the cycle progresses compared to an average cycle.
- The ranges denoted Inter-cycle variability are more appropriate to use in non-monitored cycles with only the beginning of menstruation known, but where the woman accurately knows her average cycle lengths and time of ovulation, and that they are somewhat averagely regular, with the time scale being compressed or stretched to how much a woman's average cycle length is shorter or longer, respectively, than the average of the population.
- The ranges denoted Inter-woman variability are more appropriate to use when the average cycle lengths and time of ovulation are unknown, but only the beginning of menstruation is given.