Healthcare in the United States
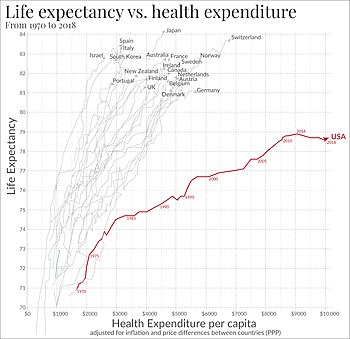
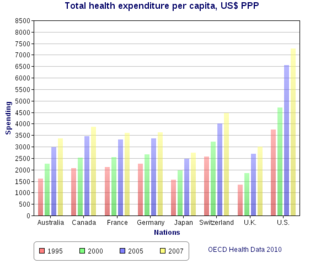
[2][3][4][5] The United States spends more on healthcare than any other country, both in absolute terms and as a percentage of GDP;[2] however, this expenditure does not necessarily translate into better overall health outcomes compared to other developed nations.
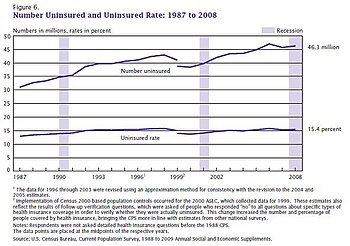
In the 21st century, the Affordable Care Act (ACA) was passed in 2010, extending healthcare coverage to millions of uninsured Americans and implementing reforms aimed at improving quality and reducing costs.
[36] A 1978 study argued that “Today every government in the world-including Red China with its squadrons of semi-trained “barefoot doctors”-realizes it has a responsibility to keep its citizens in good physical and mental health.
[65] A 2013 National Research Council study stated that, when considered as one of 17 high-income countries, the US was at or near the top in infant mortality, heart and lung disease, sexually transmitted infections, adolescent pregnancies, injuries, homicides, and rates of disability.
[86] Death certificate data from the CDC reveals that mortality rates among children and adolescents increased by 11% for the years 2019 and 2020 and a further 8% for 2020 and 2021, with injuries being a driving factor, along with homicide, suicide, drug overdoses and motor vehicle accidents impacting those aged 10 to 19.
[114] A major impending demographic shift in the US will require the healthcare system to provide more care, as the older population is predicted to increase medical expenses by 5% or more in North America[115] due to the "baby boomers" reaching retirement age.
[120] Common reasons for seeking these alternative approaches included improving their well-being, engaging in a transformational experience, gaining more control over their own health, or finding a better way to relieve symptoms caused by chronic disease.
[142] According to a study paid for by America's Health Insurance Plans (a Washington lobbyist for the health insurance industry) and carried out by PriceWaterhouseCoopers, increased utilization is the primary driver of rising healthcare costs in the US[143] The study cites numerous causes of increased utilization, including rising consumer demand, new treatments, more intensive diagnostic testing, lifestyle factors, the movement to broader-access plans, and higher-priced technologies.
[146] An analysis by the U.S. Congressional Budget Office (CBO) suggests allowing Medicare to cover weight loss drugs would raise federal spending by approximately $35 billion between 2026 and 2034.
These include the FDA, responsible for certifying the safety of food and the effectiveness of drugs and medical products; the CDC, tasked with preventing disease, premature death, and disability; the Agency for Healthcare Research and Quality, which improves the quality, safety, efficiency, and effectiveness of healthcare; the Agency for Toxic Substances and Disease Registry, which manages hazardous substance spills; and the National Institutes of Health, which conducts groundbreaking medical research.
Indirect payments and reimbursements through federal and state government programs have never fully compensated public and private hospitals for the full cost of care mandated by EMTALA.
[163] A 2019 issue brief by the Commonwealth Fund concluded that "people in the United States experience the worst health outcomes overall of any high-income nation" and that "Americans are more likely to die younger, and from avoidable causes, than residents of peer countries."
A subsequent analysis in 2022 showed a worsening of these trends, though it acknowledged that the tumultuous impact of the COVID-19 pandemic and lockdowns on healthcare in the United States was challenging to disentangle from the longer term trajectory of the system.
US healthcare tends to rely on rationing by exclusion (uninsured and underinsured), out-of-pocket costs for the insured, fixed payments per case to hospitals (resulting in very short stays), and contracts that manage demand instead.
[178] A 2014 study by the private US foundation Commonwealth Fund found that although the US healthcare system is the most expensive in the world, it ranks last on most dimensions of performance when compared with Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the UK.
[187] Another study found that the mortality gap between the well-educated and the poorly educated widened significantly between 1993 and 2001 for adults ages 25 through 64; the authors speculated that risk factors such as smoking, obesity and high blood pressure may lie behind these disparities.
[191][192] The WHO study has been criticized by the free market advocate David Gratzer because "fairness in financial contribution" was used as an assessment factor, marking down countries with high per-capita private or fee-paying health treatment.
[195] Furthermore, the relationship between patient satisfaction and healthcare utilization, expenditures, clinically meaningful measures, and the evaluation of outcomes is complex, not well defined, and only beginning to be explored.
[200] A critic of the US healthcare system, British philanthropist Stan Brock, whose charity Remote Area Medical has served over half a million uninsured Americans, stated, "You could be blindfolded and stick a pin on a map of America and you will find people in need.
The ACA is anticipated to produce an additional demand for services which the existing stable of primary care doctors will be unable to fill, particularly in economically depressed areas.
[211] A 2009 study by former Clinton policy adviser Richard Kronick published in the journal Health Services Research found no increased mortality from being uninsured after certain risk factors were controlled for.
These patients were forced to forgo necessary preventative care measures in order to save money leading to late diagnosis of easily treated diseases and more expensive procedures later.
Insurance companies and third-party disability administrators (most notably, Sedgwick CMS) used loopholes and, though providing financial equity, they often worked around the law by applying unequal copayments or setting limits on the number of days spent in inpatient or outpatient treatment facilities.
Raj Bhopal, professor emeritus at University of Edinburgh, writes that the history of racism in science and medicine shows that people and institutions behave according to the ethos of their times.
[270] Nancy Krieger, professor of social epidemiology at Harvard, wrote that racism underlies unexplained inequities in healthcare, including treatment for heart disease,[271] renal failure,[272] bladder cancer,[273] and pneumonia.
[275][276] Bhopal writes that these inequalities have been documented in numerous studies whose consistent and repeated findings were that Black Americans received less healthcare than white Americans—particularly when the care involved expensive new technology.
[278][279] The lack of equitable access to different resources is intrinsically tied to the field of public health, which works to supplement the traditional medical system with other services and opportunities.
The costs include research, design and development, meeting the U.S. Food and Drug Administration's regulatory guidelines, manufacture, marketing, distribution, and business plan.
[283] A recent scoping review identified 18 equity issues with 15 strategies to address them to try to ensure that AI applications equitably meet the needs of the populations intended to benefit from them.
[305] The Inflation Reduction Act of 2022, while still undergoing negotiations for roughly the next two years, attempts to renegotiate drug prices by amending the non-interference clause in the Medicare Part D program.