Melanoma
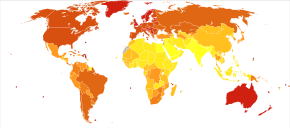
Melanoma rates tend to be highest in countries settled by migrants from Europe which have a large amount of direct, intense sunlight to which the skin of the settlers is not adapted, most notably Australia.
An alternative reading frame mutation in this gene leads to the destabilization of p53, a transcription factor involved in apoptosis and in 50% of human cancers.
This early stage of the disease is called the radial growth phase, when the tumor is less than 1 mm thick, and spreads at the level of the basal epidermis.
About 40% of human melanomas contain activating mutations affecting the structure of the B-Raf protein, resulting in constitutive signaling through the Raf to MAP kinase pathway.
If unrepaired, cyclobutane pyrimidine dimer (CPD) photoproducts can lead to mutations by inaccurate translesion synthesis during DNA replication or repair.
[59] Large-scale studies, such as The Cancer Genome Atlas, have characterized recurrent somatic alterations likely driving initiation and development of cutaneous melanoma.
[67] In another experiment they found that elasticity of melanoma cells is important for its metastasis and growth: non-pigmented tumors were bigger than pigmented and it was much easier for them to spread.
To detect melanomas (and increase survival rates), it is recommended to learn to recognize them (see "ABCDE" mnemonic), to regularly examine moles for changes (shape, size, color, itching or bleeding) and to consult a qualified physician when a candidate appears.
Following a visual examination and a dermatoscopic exam,[75] or in vivo diagnostic tools such as a confocal microscope, the doctor may biopsy the suspicious mole.
It is common for patients diagnosed with melanoma to have chest X-rays and an LDH test, and in some cases CT, MRI, and/or PET scans.
[99] Currently, newer sunscreen ingredients (avobenzone, zinc oxide, and titanium dioxide) effectively block both UVA and UVB even at lower SPFs.
[107] A 2009 meta-analysis of randomized controlled trials found a small difference in survival rates favoring wide excision of primary cutaneous melanomas, but these results were not statistically significant.
[citation needed] A process called lymphoscintigraphy is performed in which a radioactive tracer is injected at the tumor site to localize the sentinel node(s).
[119] A 2013 meta-analysis suggested that the addition of interferon alpha increased disease-free and overall survival for people with AJCC TNM stage II-III cutaneous melanoma.
[122][123] Chemotherapy drugs such as dacarbazine have been the backbone of metastatic melanoma treatment since FDA approval in 1975; however, its efficacy in terms of survival has never been proven in an RCT.
[124] Since the approval of immune checkpoint inhibitors, dacarbazine and its oral counterpart temozolomide constitute potential treatment options in later lines of therapy.
[126] In people with locally advanced cutaneous malignancies and sarcoma, isolated limb infusion (ILI) has been found to be a minimally invasive and well-tolerated procedure for delivering regional chemotherapy.
[129] These inhibitors work to inhibit the downstream pathways involved in cell proliferation and tumour development due to specific gene mutations.
[134][135] Immunotherapy is aimed at stimulating the person's immune system against the tumor, by enhancing the body's own ability to recognize and kill cancer cells.
The narrow surgical margin used, combined with the limitation of the standard "bread-loafing" technique of fixed tissue histology – result in a high "false negative" error rate, and frequent recurrences.
A meta-analysis of the literature in 2014 found no randomized controlled trials of surgical interventions to treat lentigo maligna or melanoma in-situ, even though surgery is the most widely used treatment.
[145] Some melanocytic nevi, and melanoma-in-situ (lentigo maligna) have resolved with an experimental treatment, imiquimod (Aldara) topical cream, an immune enhancing agent.
[2] The rate of melanoma has increased in the recent years, but it is not clear to what extent changes in behavior, in the environment, or in early detection are involved.
However, one example lies in a 1960s examination of nine Peruvian mummies, radiocarbon dated to be approximately 2400 years old, which showed apparent signs of melanoma: melanotic masses in the skin and diffuse metastases to the bones.
[182] Some researchers believe that combination therapies that simultaneously block multiple pathways may improve efficacy by making it more difficult for the tumor cells to mutate before being destroyed.
The study found an increase in median survival from 6.4 to 10 months in patients with advanced melanomas treated with the monoclonal ipilimumab, versus an experimental vaccine.
[191][192][193] In June 2011, a clinical trial of ipilimumab plus dacarbazine combined this immune system booster with the standard chemotherapy drug that targets cell division.
[197] Talimogene laherparepvec (T-VEC) (which is a herpes simplex virus type 1–derived oncolytic immunotherapy), was shown to be useful against metastatic melanoma in 2015 with an increased survival of 4.4 months.
[199][200] Evidence from studies on melanoma cell lines indicates that antiretroviral drugs, including lamivudine, doravirine, and cabotegravir, can effectively downregulate the expression of human endogenous retroviruses (HERV-K).
By restoring apoptosis, decreasing cell viability, and influencing tumor suppressor proteins, these antiretrovirals offer a compelling strategy to tackle therapeutic resistance in melanoma.