Meningioma
[2] Occasionally seizures, dementia, trouble talking, vision problems, one sided weakness, or loss of bladder control may occur.
[9] Atomic bomb survivors from Hiroshima had a higher than typical frequency of developing meningiomas, with the incidence increasing the closer that they were to the site of the explosion.
[11] In 2020, the European Medicine Agency issued a warning that high doses of cyproterone acetate may contribute to risk of meningioma, and to use the minimum dosage or alternative treatment for most indications, with the exception of prostate carcinoma.
Some subtypes may arise from the pial cap cells that migrate during the development together with blood vessels into the brain parenchyma.
[citation needed] Other uncommon locations are the lateral ventricle, foramen magnum, and the orbit/optic nerve sheath.
[citation needed] Histologically, meningioma cells are relatively uniform, with a tendency to encircle one another, forming whorls and psammoma bodies (laminated calcific concretions).
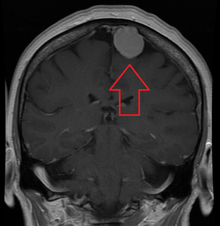
[citation needed] On T1-weighted contrast-enhanced MRI, they may show a typical dural tail sign absent in some rare forms of meningiomas.
[26] Even if, by general rule, neoplasms of the nervous system (brain tumors) cannot metastasize into the body because of the blood–brain barrier, anaplastic meningioma can.
Although they are inside the cerebral cavity, they are located on the bloodside of the BBB, because meningiomas tend to be connected to blood vessels.
[27] The risk of meningioma can be reduced by maintaining a normal body weight,[28] and by avoiding unnecessary dental x-rays.
[30] In this study, younger patients were found to have tumors that were more likely to have grown on repeat imaging; thus are poorer candidates for observation.
[32] Meningiomas usually can be surgically resected (removed) and result in a permanent cure if the tumor is superficial on the dural surface and easily accessible.
[35] Fractionated external-beam radiation also can be used as primary treatment for tumors that are surgically unresectable or, for patients who are inoperable for medical reasons.
[citation needed] Radiation therapy often is considered for WHO grade I meningiomas after subtotal (incomplete) tumor resections.
The clinical decision to irradiate after a subtotal resection is somewhat controversial, as no class I randomized, controlled trials exist on the subject.
[37] In the case of a grade III meningioma, the current standard of care involves postoperative radiation treatment regardless of the degree of surgical resection.
Grade II tumors may behave variably and there is no standard of whether to give radiotherapy following a gross total resection.
With the advent of modern sophisticated imaging systems such as CT scans, the discovery of asymptomatic meningiomas has tripled.
[citation needed] The modern term of "meningioma" was used first by Harvey Cushing (1869–1939) in 1922, to describe a set of tumors that occur throughout the neuraxis (brain and spinal cord), but have various commonalities.
[citation needed] The earliest written record of what was probably a meningioma is from the 1600s, when Felix Plater (1536–1614) of the University of Basel performed an autopsy on Sir Caspar Bonecurtius.
[43] The first documented successful removal of a skull base meningioma was performed in 1835 by Zanobi Pecchioli, Professor of Surgery at the University of Siena.
[41] Improvements in meningioma research and treatment over the last century have occurred in terms of the surgical techniques for removal of the tumor, and related improvements in anesthesia, antiseptic methods, techniques to control blood loss, better ability to determine which tumors are and are not operable,[44] and to effectively differentiate between the different meningioma subtypes.


- A woven architectural pattern
- Psammoma bodies (spheroid calcifications)
- Syncytial cells (having indistinct cell membranes) with eosinophilic (pink) cytoplasms
- Round uniform nuclei
- Whorls (concentric cell arrangements) [ 16 ]