Methylprednisolone
[7] Regardless of the route of administration, methylprednisolone integrates systemically as exhibited by its effectiveness to quickly reduce inflammation during acute flares.
[9] Serious side effects include iatrogenic Cushing's syndrome, hypertension, osteoporosis, diabetes, infection, and skin atrophy.
[15] For exacerbations that result in a visit to the Emergency Department (ED), oral methylprednisolone is preferred over intravenous administration, unless there are issues with adherence or vomiting.
[15][16] Dosage above 60–80 mg/day or 2 mg/kg/day is not recommended as it has not been shown to alter pulmonary function, rate of admission, or length of stay in the hospital compared to lower doses.
[15][16] Methylprednisolone is used to treat several rheumatic diseases, such as Systemic Lupus Erythematosus (SLE) and Rheumatoid Arthritis (RA).
Severe manifestations are often treated with Cyclophosphamide or Rituximab and three doses of methylprednisolone IV-pulse treatment (as recommended by ACR guidelines) before switching to oral prednisolone and azathioprine for maintenance.
[17][18] Intra-articular corticosteroid injections (IACI) are a second-line therapy to relieve joint pain resulting from rheumatoid arthritis.
[20] Methylprednisolone is not typically recommended for primary or secondary adrenocortical insufficiency compared to other corticosteroids which have a higher affinity for mineralocorticoid receptors and salt-retaining properties.
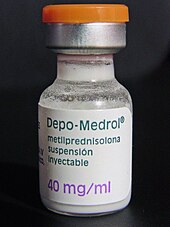
2Benzyl alcohol should not be used on neonates 3Preservative free formulation Methylprednisolone should not be taken orally by people who have systemic fungal infections, except for Depo-Medrol when administered as an intra-articular injection for localized joint conditions.
[22] Severe medical events have been associated with epidural administration of Solu-Medrol and Depo-Medrol, including spinal cord infarction, paraplegia, quadriplegia, cortical blindness and stroke.
[22] Exposure of neural tissue to excessive amounts of benzyl alcohol has been associated with toxicity and in rare events has resulted in death.
[9] There is minimal clinical diagnostic criteria to define the psychic adverse effects (PAE) associated with methylprednisolone use in patients with systemic lupus erythematosus (SLE).
[25] Traditional symptoms include weight gain, myopathy, osteoporosis, increased risk of infection, hypertension, and psychological effects.
[25] The onset of side effects varies; neuropsychiatric symptoms can arise within a few hours, while osteoporosis takes months to develop.
[25] The metabolic effects of taking methylprednisolone involve the continuous breakdown of proteins for gluconeogenesis increasing the necessity for insulin.
[26] The World Health Organization (WHO) defines osteoporosis in caucasian postmenopausal women as a bone mineral density (BMD) and a T-score of -2.5 or less.
[27] Additionally, a UK-based study showed that BMD may underrepresent a patient with SLE, as their risk for fractures is 22% higher than the healthy individual.
[25] Dermatologic: impaired wound healing, petechiae, and ecchymoses, thinning of the skin, facial erythema, and increased sweating.
[21] Endocrine: Cushingoid features, growth suppression in children, secondary adrenocortical and pituitary unresponsiveness, menstrual irregularities, decreased carbohydrate intolerance, and latent diabetes mellitus.
[9][29] Factors that contribute to the extent of HPA axis suppression include steroid hormone potency (type of compound and route of administration), cumulative dose, duration of treatment and concomitant drug use.
[32] Phenobarbital, phenytoin, rifampin, carbamazepine and barbiturates, increase hepatic enzymes and rate of elimination, thus reducing the immunosuppressive effect of methylprednisolone.
[32] Methylprednisolone and cyclosporin inhibit metabolism and therefore increase the likelihood of experiencing side effects associated with either of the individual drugs.
[6] In the absence of endogenous or synthetic GCs, monomeric GRs are located in the cytoplasm and form multiprotein complexes with heat shock proteins (HSPs), immunophilins, and other chaperones such as src, and p23.
[6] When methylprednisolone from the plasma or interstitial fluid diffuses passively across the cell membrane, it binds to the GR inducing a conformational change and GC-GR dimerization.
[5] One mechanism of genomic signaling occurs when the MP-GR complex directly binds to DNA sequences called glucocorticoid response elements (GREs).
[6][34] PTMs modulate many functions including nuclear translocation, strength and duration of receptor signaling and cofactor interaction.
[37][27] It is evidence that dissociated SRC is responsible for inhibiting the release of arachidonic acid (AA) from cell membrane phospholipids.
ATP consumption drops (resembled by inhibited respiration), resulting in protein permeability at the inner mitochondrial membrane and uncoupling of oxidative phosphorylation.
[23] Solu-Medrol is the only derivative of methylprednisolone that is approved for intravenous infusion, as the sterile powder is soluble in water and can be mixed with a diluent.
[4] Methylprednisolone was first synthesized and manufactured by The Upjohn Company (now Pfizer) and Food and Drug Administration (FDA) approved in the United States in October 1957.